Structural and functional elements tissues are divided into: histological elements cellular (1) and non-cellular type (2). Structural and functional elements of the tissues of the human body can be compared with different threads that make up textile fabrics.
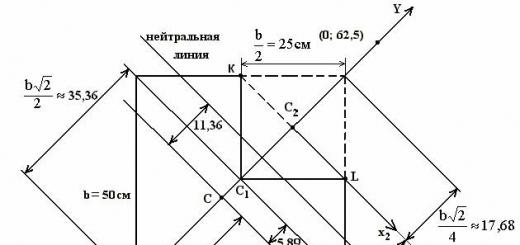
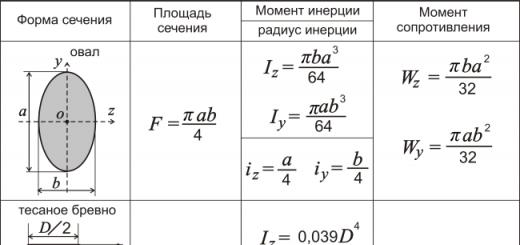
Histological preparation "Hyaline cartilage": 1 - chondrocyte cells, 2 - intercellular substance (a histological element of non-cellular type)
1. Histological elements of the cell type are usually living structures with their own metabolism, limited by the plasma membrane, and are cells and their derivatives resulting from specialization. These include:
a) Cells- the main elements of tissues that determine their basic properties;
b) Postcellular structures in which the most important signs for cells (nucleus, organelles) are lost, for example: erythrocytes, horny scales of the epidermis, as well as platelets, which are parts of cells;
in) Symplasts- structures formed as a result of the fusion of individual cells into a single cytoplasmic mass with many nuclei and a common plasma membrane, for example: skeletal muscle tissue fiber, osteoclast;
G) syncytia- structures consisting of cells united in a single network by cytoplasmic bridges due to incomplete separation, for example: spermatogenic cells at the stages of reproduction, growth and maturation.
2. Histological elements of non-cellular type are represented by substances and structures that are produced by cells and released outside the plasmalemma, united under the general name "intercellular substance" (tissue matrix). intercellular substance usually includes the following varieties:
a) Amorphous (basic) substance – represented by a structureless accumulation of organic (glycoproteins, glycosaminoglycans, proteoglycans) and inorganic (salts) substances located between tissue cells in a liquid, gel-like or solid, sometimes crystallized state (the main substance of bone tissue);
b) fibers – consist of fibrillar proteins (elastin, various types of collagen), often forming bundles of different thicknesses in an amorphous substance. Among them are distinguished: 1) collagen, 2) reticular and 3) elastic fibers. Fibrillar proteins are also involved in the formation of cell capsules (cartilage, bones) and basement membranes (epithelium).
 The photo shows a histological preparation "Loose fibrous connective tissue": cells are clearly visible, between which the intercellular substance (fibers - strips, amorphous substance - light areas between cells).
The photo shows a histological preparation "Loose fibrous connective tissue": cells are clearly visible, between which the intercellular substance (fibers - strips, amorphous substance - light areas between cells).
2. Classification of fabrics. In accordance with morphofunctional classification tissues are distinguished: 1) epithelial tissues, 2) tissues of the internal environment: connective and hematopoietic, 3) muscle and 4) nervous tissue.
3. Development of tissues. The theory of divergent development fabrics according to N.G. Khlopin suggests that tissues arose as a result of divergence - a divergence of signs in connection with the adaptation of structural components to new conditions of functioning. Theory of parallel series according to A.A. Zavarzin describes the reasons for the evolution of tissues, according to which tissues that perform similar functions have a similar structure. In the course of phylogenesis, identical tissues arose in parallel in different evolutionary branches of the animal world, i.e. completely different phylogenetic types of original tissues, falling into similar conditions for the existence of an external or internal environment, gave similar morphofunctional types of tissues. These types arise in phylogeny independently of each other, i.e. in parallel, in absolutely different groups of animals under the same circumstances of evolution. These two complementary theories are combined into a single evolutionary concept of tissues(A.A. Braun and P.P. Mikhailov), according to which similar tissue structures in different branches of the phylogenetic tree arose in parallel during divergent development.
How can such a variety of structures be formed from one cell - a zygote? Such processes as DETERMINATION, COMMITMENT, DIFFERENTIATION are responsible for this. Let's try to understand these terms.
determination- This is a process that determines the direction of development of cells, tissues from embryonic rudiments. In the course of determination, cells get the opportunity to develop in a certain direction. Already in the early stages of development, when crushing occurs, two types of blastomeres appear: light and dark. From light blastomeres, for example, cardiomyocytes and neurons cannot subsequently be formed, since they are determined and their direction of development is the chorionic epithelium. These cells have very limited opportunities (potency) to develop.
Stepwise, consistent with the program of development of the organism, the restriction of possible development paths due to determination is called committing . For example, if cells of the primary ectoderm in a two-layer embryo can still develop cells of the renal parenchyma, then with further development and formation of a three-layer embryo (ecto-, meso- and endoderm) from the secondary ectoderm, only nervous tissue, epidermis of the skin and some other things.
The determination of cells and tissues in the body, as a rule, is irreversible: mesoderm cells that have moved out of the primary streak to form the renal parenchyma will not be able to turn back into primary ectoderm cells.
Differentiation is aimed at creating several structural and functional cell types in a multicellular organism. In humans, there are more than 120 such cell types. In the course of differentiation, the gradual formation of morphological and functional signs of specialization of tissue cells (formation of cell types) occurs.
Differon is a histogenetic series of cells of the same type at different stages of differentiation. Like people on the bus - children, youth, adults, the elderly. If a cat and kittens are transported on the bus, then we can say that there are “two diferons” on the bus - people and cats.
As part of Differon, the following cell populations are distinguished according to the degree of differentiation: a) stem cells- the least differentiated cells of a given tissue, capable of dividing and being a source of development of its other cells; b) semi-stem cells- precursors have limitations in their ability to form different types of cells due to commitment, but are capable of active reproduction; in) cells are blasts that have entered into differentiation but retain the ability to divide; G) maturing cells- completing differentiation; e) mature(differentiated) cells that complete the histogenetic series, the ability to divide in them, as a rule, disappears, they actively function in the tissue; e) old cells- completed active operation.
The level of cell specialization in differon populations increases from stem cells to mature cells. In this case, changes in the composition and activity of enzymes, cell organelles occur. The histogenetic series of differon is characterized by principle of irreversibility of differentiation, i.e. under normal conditions, the transition from a more differentiated state to a less differentiated state is impossible. This property of differon is often violated in pathological conditions (malignant tumors).
An example of differentiation of structures with the formation of a muscle fiber (successive stages of development).
Zygote - blastocyst - inner cell mass (embryoblast) - epiblast - mesoderm - unsegmented mesoderm- somite - somite myotome cells- mitotic myoblasts - postmitotic myoblasts - muscular tube - muscle fiber.
In the above scheme, from stage to stage, the number of potential directions of differentiation is limited. Cells unsegmented mesoderm have the ability (potency) to differentiate in various directions and the formation of myogenic, chondrogenic, osteogenic and other directions of differentiation. Somite myotome cells are determined to develop in only one direction, namely, to the formation of a myogenic cell type (striated muscle of the skeletal type).
Cell populations is a collection of cells of an organism or tissue that are similar to each other in some way. According to the ability to self-renewal by cell division, 4 categories of cell populations are distinguished (according to Leblon):
- Embryonic(rapidly dividing cell population) - all cells of the population are actively dividing, specialized elements are absent.
- stable cell population - long-lived, actively functioning cells, which, due to extreme specialization, have lost the ability to divide. For example, neurons, cardiomyocytes.
- Growing(labile) cell population - specialized cells of which are able to divide under certain conditions. For example, the epithelium of the kidney, liver.
- Upgrading population consists of cells that are constantly and rapidly dividing, as well as specialized functioning descendants of these cells, the lifespan of which is limited. For example, intestinal epithelium, hematopoietic cells.
A special type of cell populations are clone- a group of identical cells derived from a single ancestral progenitor cell. concept clone as a cell population is often used in immunology, for example, a clone of T-lymphocytes.
4. Tissue regeneration- a process that ensures its renewal during normal life (physiological regeneration) or recovery after damage (reparative regeneration).
cambial elements - these are populations of stem, semi-stem progenitor cells, as well as blast cells of a given tissue, the division of which maintains the required number of its cells and replenishes the decline in the population of mature elements. In those tissues in which cell renewal does not occur by cell division, the cambium is absent. According to the distribution of cambial tissue elements, several varieties of cambium are distinguished:
- Localized cambium– its elements are concentrated in specific areas of the tissue, for example, in the stratified epithelium, the cambium is localized in the basal layer;
- Diffuse cambium– its elements are dispersed in the tissue, for example, in smooth muscle tissue, cambial elements are dispersed among differentiated myocytes;
- Exposed cambium- its elements lie outside the tissue and, as they differentiate, are included in the composition of the tissue, for example, blood contains only differentiated elements, cambium elements are located in the hematopoietic organs.
The possibility of tissue regeneration is determined by the ability of its cells to divide and differentiate or the level of intracellular regeneration. Tissues that have cambial elements or are renewing or growing cell populations regenerate well. The activity of division (proliferation) of cells of each tissue during regeneration is controlled by growth factors, hormones, cytokines, kalons, as well as the nature of functional loads.
In addition to tissue and cellular regeneration through cell division, there is intracellular regeneration- the process of continuous renewal or restoration of the structural components of the cell after their damage. In those tissues that are stable cell populations and lack cambial elements (nervous tissue, cardiac muscle tissue), this type of regeneration is the only possible way to renew and restore their structure and function.
tissue hypertrophy- an increase in its volume, mass and functional activity - is usually a consequence of a) cell hypertrophy(with their number unchanged) due to enhanced intracellular regeneration; b) hyperplasia - increase in the number of its cells by activating cell division ( proliferation) and (or) as a result of accelerating the differentiation of newly formed cells; c) combinations of both processes. tissue atrophy- a decrease in its volume, mass and functional activity due to a) atrophy of its individual cells due to the predominance of catabolism processes, b) the death of some of its cells, c) a sharp decrease in the rate of cell division and differentiation.
5. Intertissue and intercellular relationships. The tissue maintains the constancy of its structural and functional organization (homeostasis) as a single whole only under the constant influence of histological elements on each other (interstitial interactions), as well as one tissue on another (intertissue interactions). These influences can be considered as processes of mutual recognition of elements, formation of contacts and exchange of information between them. In this case, a variety of structural-spatial associations are formed. Cells in a tissue can be at a distance and interact with each other through the intercellular substance (connective tissues), come into contact with processes, sometimes reaching a considerable length (nervous tissue), or form tightly contacting cell layers (epithelium). The totality of tissues united into a single structural whole by connective tissue, the coordinated functioning of which is ensured by nervous and humoral factors, forms organs and organ systems of the whole organism.
For the formation of tissue, it is necessary for the cells to unite and be interconnected in cellular ensembles. The ability of cells to selectively attach to each other or to the components of the intercellular substance is carried out using the processes of recognition and adhesion, which are a necessary condition for maintaining the tissue structure. Recognition and adhesion reactions occur as a result of the interaction of macromolecules of specific membrane glycoproteins, called adhesion molecules. Attachment occurs with the help of special subcellular structures: a ) point adhesive contacts(attachment of cells to the intercellular substance), b) intercellular connections(attachment of cells to each other).
Intercellular connections- specialized structures of cells, with the help of which they are mechanically fastened together, and also create barriers and permeability channels for intercellular communication. Distinguish: 1) adhesive cell junctions, performing the function of intercellular adhesion (intermediate contact, desmosome, semi-desmasome), 2) make contacts, whose function is the formation of a barrier that traps even small molecules (tight contact), 3) conductive (communication) contacts, whose function is to transmit signals from cell to cell (gap junction, synapse).
6. Regulation of vital activity of tissues. Tissue regulation is based on three systems: nervous, endocrine and immune. Humoral factors that provide intercellular interaction in tissues and their metabolism include a variety of cellular metabolites, hormones, mediators, as well as cytokines and chalones.
Cytokines are the most versatile class of intra- and interstitial regulatory substances. They are glycoproteins that, at very low concentrations, influence the reactions of cell growth, proliferation and differentiation. The action of cytokines is due to the presence of receptors for them on the plasmolemma of target cells. These substances are carried by the blood and have a distant (endocrine) action, and also spread through the intercellular substance and act locally (auto- or paracrine). The most important cytokines are interleukins(IL), growth factors, colony stimulating factors(KSF), tumor necrosis factor(TNF), interferon. Cells of various tissues have a large number of receptors for various cytokines (from 10 to 10,000 per cell), the effects of which often overlap, which ensures high reliability of the functioning of this system of intracellular regulation.
Keylons– hormone-like regulators of cell proliferation: inhibit mitosis and stimulate cell differentiation. Keylons act on the principle of feedback: with a decrease in the number of mature cells (for example, loss of the epidermis due to trauma), the number of keyons decreases, and the division of poorly differentiated cambial cells increases, which leads to tissue regeneration.
The concept of tissues.Types of fabrics.
Structure and functions
epithelial tissue.
The concept and types of tissues
Tissue is a system of cells similar inorigin, structure and
functions and intercellular (tissue)
liquid.
The study of tissues is called
histology (Greek histos - tissue, logos
- teaching). Types of fabrics:
-epithelial
or coverslip
-connective
i (tissue
internal
environment);
- muscular
- nervous
epithelial tissue
Epithelial tissue (epithelium) istissue that covers the surface of the skin
eye, as well as lining all cavities
body, inner surface
hollow digestive organs
respiratory, urinary systems,
found in most glands
organism. Distinguish between cover and
glandular epithelium.
Functions of the epithelium
IntegumentaryProtective
excretory
Provides mobility
internal organs in serous
cavities
Epithelium classification:
Single layer:flat - endothelium (all vessels from the inside) and
mesothelium (all serous membranes)
cuboidal epithelium (renal tubules,
salivary gland ducts)
prismatic (stomach, intestines, uterus,
fallopian tubes, bile ducts)
cylindrical, ciliated and ciliated
(intestine, respiratory tract)
Glandular (single or multilayer)
Classification of the epithelium
Multilayer:flat
keratinizing (epidermis
skin) and non-keratinizing (mucous
membranes, cornea of the eye) - are
integumentary
transition
- in the urinary tract
structures: renal pelvis, ureters,
bladder, the walls of which
highly stretchable
Connective tissue. Structural features.
Connective tissue is made up of cells anda large amount of intercellular substance,
including the main amorphous substance and
Connective tissue.
fibers.
Featuresfabric
buildings.
Connective
is a tissue
internal environment, does not come into contact with the external
environment and body cavities.
Participates in the construction of all internal
organs.
Connective tissue functions:
mechanical, supporting and shaping,makes up the supporting system of the body: bones
skeleton, cartilage, ligaments, tendons, forming
capsule and stroma of organs;
protective, carried out by
mechanical protection (bones, cartilage, fascia),
phagocytosis and production of immune bodies;
trophic, associated with the regulation of nutrition,
metabolism and maintenance of homeostasis;
plastic, expressed in active
participation in wound healing processes.
Connective tissue classification:
Connective tissue proper:Loose fibrous connective tissue (surrounds
blood vessels, organ stroma)
Dense fibrous connective tissue is formed
(ligaments, tendons, fascia, periosteum) and unformed
(mesh layer of skin)
With special features:
adipose - white (in adults) and brown (in newborns), lipocyte cells
reticular (BCM, lymph nodes, spleen),
reticular cells and fibers
pigmented (nipples, scrotum, around the anus,
iris, moles), cells - pigmentocytes Skeletal connective tissue:
Cartilaginous: chondroblasts, chondrocytes, collagen and
elastic fibers
hyaline (articular cartilage, costal, thyroid
cartilage, larynx, bronchi)
elastic (epiglottis, auricle, auditory
pass)
fibrous (intervertebral discs, pubic
symphysis, meniscus, joint mandible, sternoclavicular joint)
Bone:
coarse-fibred (in the embryo, in the sutures of the skull of an adult)
lamellar (all human bones)
Muscle
striated muscle tissue - all skeletalmusculature. It consists of long multi-core
cylindrical threads capable of contraction, and their ends
end in tendons. SFU - muscle fiber
Smooth muscle tissue - found in the walls of hollow
organs, blood and lymph vessels, skin and
choroid of the eyeball. The cut is smooth
muscle tissue is not subject to our will.
Cardiac striated muscle tissue
cardiomyocytes are small, with one or two nuclei,
abundance of mitochondria, do not end in tendons, have
special contacts - nexuses for the transmission of impulses. Not
regenerate
nervous tissue
The main functional propertynervous tissue is excitability and
conduction (transmission of impulses). She is
capable of receiving stimuli from
external and internal environment and transfer
them along their fibers to other tissues and
body organs. Nervous tissue is made up of
neurons and support cells
neuroglia. Neurons are
polygonal cells with
processes along which
impulses. depart from the body of neurons
shoots of two types. The longest of
them (single), conductive
irritation from the body of the neuron - the axon.
Short branching shoots
which impulses are conducted along
towards the body of the neuron are called
dendrites (Greek dendron - tree).
Types of neurons by the number of processes
unipolar - with one axon, rarelymeet
pseudo-unipolar - whose axon and dendrite
start from the general outgrowth of the cell body with
subsequent T-shaped division
bipolar - with two processes (axon and
dendrite).
multipolar - more than 2 processes
Types of neurons by function:
afferent (sensory) neurons- carry impulses from receptors to reflex
center.
intercalary (intermediate) neurons
-carry out communication between neurons.
efferent (motor) neurons transmit impulses from the CNS to effectors
(executive bodies).
neuroglia
Neuroglia from allsides surrounds
neurons and makes up
stroma of the CNS. cells
neuroglia 10 times
more than
neurons, they can
share. neuroglia
is about 80%
brain masses. She is
performs in the nervous
support fabric,
secretory,
trophic and
protective function.
Nerve fibers
these are processes (axons) of nerve cells, usually coveredshell. A nerve is a collection of nerve fibers
enclosed in a common connective tissue sheath.
The main functional property of nerve fibers
is the conductivity. Depending on the building
Nerve fibers are divided into myelinated (pulp) and
unmyelinated (meelless). At regular intervals
the myelin sheath is interrupted by nodes of Ranvier.
This affects the rate of excitation
nerve fibre. In myelin fibers, excitation
transmitted abruptly from one interception to another with
high speed, reaching 120 m / s. AT
unmyelinated fibers excitation transfer rate
does not exceed 10 m/s.
Synapse
From (Greek synaps - connection, connection) - connection betweenpresynaptic axon ending and membrane
postsynaptic cell. In any synapse, there are three
main parts: presynaptic membrane, synaptic
cleft and postsynaptic membrane.
Lugansk National Agrarian University
Cytology, embryology, general histology
(lecture course)
Lugansk - 2005
Cytology, embryology, general histology
The course of lectures was compiled by the head of the Department of Animal Biology, Doctor of Biological Sciences, Professor G.D. Katsy.
2nd edition, revised and enlarged.
Lectures are prepared for students of zoobiotechnological and faculty of veterinary medicine of Lugansk National Agrarian University. I sincerely thank the postgraduate student of the Department of Animal Biology Krytsya Ya.P. and head of the laboratory Esaulenko V.P. for their help in preparing the material for publication.
Introduction to histology
1. The subject of histology and its place in the system of biological and veterinary sciences.
2. History and methods of microscopic research.
3. Cell theory, basic provisions.
1. The specificity of agricultural production is due to the fact that, despite the increasing role of technical factors, biological objects remain the main tools and means of production. According to the scope of the objects of study and in its depth, veterinary medicine is: as Academician K.I. Skryabin said, the most interesting field of human knowledge: in which so many representatives of the animal kingdom are investigated and protected.
Cytology, histology and embryology, along with physiology, biochemistry and other sciences, form the foundation of modern veterinary medicine.
Histology (Greek histos-tissue, logos-teaching) is the science of the development, structure and vital activity of tissues of animal organisms. Modern histology studies the structures of the organisms of animals and humans in connection with the processes occurring in them, reveals the relationship between function and structure, etc.
Histology is divided into 3 main sections: cytology, or the study of the cell; embryology, or the study of the embryo; and general and particular histology, or the study of tissues, the microscopic structure of organs, their cellular and tissue composition.
Histology is closely related to a number of biological and veterinary sciences - general and comparative anatomy, physiology, pathological physiology and pathological anatomy, as well as some clinical disciplines (internal medicine, obstetrics and gynecology, etc.).
Future doctors need a good knowledge of the structure of cells and tissues of organs, which are the structural basis of all types of vital activity of the body. The importance of histology, cytology, and embryology for doctors is also increasing because modern veterinary medicine is characterized by the widespread use of cytological and histological methods in blood tests, bone marrow, organ biopsies, etc.
2. The concept of tissue was first introduced into biology by the brilliant young French anatomist and physiologist Xavier Bichat (Bichat, 1771-1802), who was so impressed by the varied texture of the various layers and structures that he discovered in anatomical studies that he wrote a book on tissues of the body, giving in it the name of more than 20 of their species.
The term “histology” does not belong to Bish, although he can be considered the first histologist. The term "histology" 17 years after Bisha's death was proposed by the German researcher Meyer.
A tissue is a phylogenetically determined elementary system united by a common structure, function and development (A.A. Zavarzin).
The successes of histology from the moment of its inception to the present are primarily associated with the development of technology, optics and microscopy methods. The history of histology can be divided into three periods: 1st - pre-microscopic (about 2000 years), 2nd - microscopic (about 300 years), 3rd - electron microscopic (about 40 years).
In modern histology, cytology and embryology, a variety of research methods are used to comprehensively study the processes of development, structure and function of cells, tissues and organs.
The objects of study are living and dead (fixed) cells and tissues, their images obtained in light and electron microscopes or on a television screen. There are a number of methods that allow the analysis of these objects:
1) methods for studying living cells and tissues: a) life-time study of cells in the body (in vivo) - using the methods of implanting transparent chambers into the body of animals, by transplantation;
b) the study of living structures in cell and tissue culture (in vitro) - disadvantages: the relationship with other cells and tissues is lost, the effect of a complex of neurohumoral regulatory factors, and more;
c) vital and supravital staining, i.e. intravital staining and staining of living cells isolated from the body.
2) examination of dead cells and tissues; the main object of study here are histological preparations prepared from fixed structures.
The process of making a histological preparation for light and electron microscopy includes the following main steps: 1) taking the material and fixing it, 2) compacting the material, 3) preparing sections, 4) staining or color contrasting. For light microscopy, one more step is necessary - enclosing the sections in a balm or other transparent media (5).
3) study of the chemical composition and metabolism of cells and tissues:
Cyto- and histochemical methods,
Radio autography method, which is based on the use of radioactive elements (for example, phosphorus-32P, carbon -14C, sulfur-35S, hydrogen-3H) or compounds labeled with it.
Differential centrifugation method - the method is based on the use of centrifuges, giving from 20 to 150 thousand revolutions per minute. At the same time, various components of cells are separated and precipitated and their chemical composition is determined. - interferometry - the method allows to estimate the dry mass and concentration of dense substances in living and fixed cells. - quantitative histochemical methods - cytospectrophotometry - a method of quantitative study of intracellular substances by their absorption properties. Cytospectrofluorometry is a method for studying intracellular substances by their fluorescence spectra.
4) methods of immunofluorescent analysis. They are used to study the processes of cell differentiation, to identify specific chemical compounds and structures. They are based on antigen-antibody reactions.
Methods of microscopy of histological preparations:
Light microscopy: a) ultraviolet, b) fluorescent (luminescent).
Electron microscopy: a) transmission, b) scanning (reading). The first gives only a planar image, the second - a spatial one; the main advantage of the latter (raster) is a large depth of field (100-1000 times greater than that of light microscopes), a wide range of continuous changes in magnification (from tens to tens of thousands of times) and high resolution.
3. The organism of higher animals consists of microscopic elements - cells and a number of their derivatives - fibers, amorphous matter.
The value of a cell in a multicellular organism is determined by what is transmitted through it hereditary information, the development of multicellular animals begins with it; due to the activity of cells, non-cellular structures and the ground substance are formed, which, together with cells, form tissues and organs that perform specific functions in a complex organism. Dutrochet (1824, 1837) and Schwann (1839) should be considered the creator of the cell theory.
Dutrochet (1776-1847) - zoologist, botanist, morphologist, physiologist. In 1824 he published his book Anatomical and Physiological Investigations on the Fine Structure of Animals and Plants and Their Motility.
The creation of the cell theory was preceded by the following discoveries. In 1610, the 46-year-old prof. mathematician of the University of Padua G. Galileo designed a microscope. In 1665, Robert Hooke discovered the cell at 100x magnification. His contemporary, Felice Fontana, said: “”... Everyone can look through a microscope, but only a few can judge what they see.” “Micrography” of Hooke included 54 observations, including “Observation 18. On the schematism or structure of cork, or on cells and pores in some other loose bodies.”
From the history. A company of young people (students) living in London in 1645 began to meet every day after classes to discuss the problems of experimental philosophy. Among them were Robert Boyle (18 years old), R. Hooke (17 years old), Ren (23 years old) and others. This is how the British Academy was born, then the Royal Society of London (Charles II was its honorary member).
The animal cell was discovered by Anton van Leeuwenhoek (1673-1695). He lived in Delft and traded in cloth. He brought his microscopes up to 275 x. Peter I showed blood circulation in the tail of an eel larva.
Currently, the cell theory says: 1) the cell is the smallest unit of the living, 2) cells different organisms are similar in structure, 3) cell reproduction occurs by dividing the original cell, 4) multicellular organisms are complex ensembles of cells and their derivatives, combined into integral integrated systems of tissues and organs, subordinate and interconnected by intercellular, humoral and nervous forms of regulation.
Cell - the elementary unit of life
1. Composition and physicochemical characteristics living substance.
2. Types of cells. Theories of the origin of the eukaryotic cell.
3. Cell membranes, their molecular composition and functions.
1. A typical cell with a nucleus, cytoplasm and all the organelles contained in it cannot yet be considered the smallest unit of living matter, or protoplasm (Greek “protos” - the first, “plasma” - formation). There are also more primitive or more simply organized units of life - the so-called prokaryotic organisms (Greek "karyon" - core), which include most viruses, bacteria and some algae; they, unlike cells of a higher type with a real nucleus (eukaryotic cells), lack a nuclear membrane and the nuclear substance mixes or directly comes into contact with the rest of the protoplasm.
The composition of living matter includes proteins, nucleic acids (DNA and RNA), polysaccharides and lipids. The chemical components of a cell can be divided into inorganic (water and mineral salts) and organic (proteins, carbohydrates, nucleic acids, lipids, etc.).
The cytoplasm of plant and animal cells contains 75-85% water, 10-20% protein, 2-3% lipids, 1% carbohydrates and 1% inorganic substances.
DNA is a molecule (it contains 0.4%) that contains genetic information that directs the synthesis of specific cellular proteins. For one DNA molecule, there are about 44 RNA molecules, 700 protein molecules and 7000 lipid molecules.
The primary structure of RNA is similar to that of DNA, except that RNA contains ribose and uracil instead of thymine. It has now been established that there are three types of RNA differing in molecular weight and other properties: ribosomal, informational, and transport. These three types of RNA are synthesized in the nucleus and are involved in protein synthesis.
2. Shutton (1925) divided all living organisms into two types (klisters) - prokaryotes and eukaryotes. They diverged in the Precambrian (600-4500 million years ago). There are two concepts of the origin of the eukaryotic cell: exogenous (symbiotic) and endogenous. The first is based on the recognition of the principle of combining different prokaryotic organisms with each other. The endogenous concept is based on the principle of direct filiation, i.e. sequential evolutionary transformation of prokaryotic organisms into eukaryotic ones.
In the mammalian body, histologists list about 150 types of cells, and most of them are adapted to perform one specific task. The shape and structure of the cell depends on the function it performs.
Cell functions: irritability, contractility, secretion, respiration, conduction, absorption and assimilation, excretion, growth and reproduction.
3. Any cell is delimited by a plasma membrane. It is so thin that it cannot be seen under a light microscope. The plasma membrane, easily damaged by a microneedle, is capable of recovery, but with more severe damage, especially in the absence of calcium ions, the cytoplasm flows out through the puncture and the cell dies.
According to current theory, the plasma membrane consists of a bilayer of polar lipids and globular protein molecules embedded in it. Thanks to these layers, the membrane has elasticity and relative mechanical strength. The plasma membrane of most cell types consists of three layers approximately 2.5 nm wide each. A similar structure, called the “elementary membrane,” is also found in most intracellular membranes. Biochemical analysis showed that lipids and proteins are contained in them in a ratio of 1.0: 1.7. The protein component, called stromatin, is an acidic fibrillar protein with a high molecular weight. The bulk of the lipid components are formed by phospholipids, mainly lecithin and cephalin.
The plasmalemma is a cell membrane that performs delimiting, transport and receptor functions. It provides mechanical communication of cells and intercellular interactions, contains cellular receptors for hormones and other signals of the environment surrounding the cell, transports substances into the cell from the cell both along the concentration gradient - passive transfer, and with energy costs against the concentration gradient - active transfer.
The shell consists of a plasma membrane, a non-membrane complex - glycocalex and a submembrane musculoskeletal apparatus.
The glycocalex contains about 1% carbohydrates, the molecules of which form long branching chains of polysaccharides associated with membrane proteins. Proteins located in the glycocalex - enzymes are involved in the final extracellular breakdown of substances. The products of these reactions in the form of monomers enter the cell. With active transfer, the transport of substances into the cell is carried out either by the entry of molecules in the form of a solution - pinocytosis, or by the capture of large particles - phagocytosis.
In accordance with the functional and morphological features of tissues, the cell membrane forms the apparatus of intercellular contacts characteristic of them. Their main forms are: simple contact (or sticking zone), tight (closing) and gap contact. Desmosomes are a type of tight contact.
Biological membranes act as diffuse barriers. Due to their selective permeability for K+, Na+, Cl-, etc. ions, as well as macromolecular compounds, they delimit intra- and intercellular reaction zones and create electrical and substance concentration gradients. This makes possible the existence of ordered biological structures with specific functions.
The entry of substances into a cell is called endocytosis. But there is also exocytosis. For example, secretory vesicles are laced from the Golgi apparatus, migrating towards the cell membrane and throwing their contents out. In this case, the vesicle membrane merges with the cell membrane homologous to it.
Based on electron microscopic data, it can be assumed that the plasma membrane is a product of the Golgi apparatus. From this organelle, in the form of continuously separating vesicles, there is a constant transport of membrane material (“membrane flow”), which restores the used sections of the plasmolemma and ensures its growth after cell division.
The membrane is a carrier of species-specific and cell-specific surface properties associated with the characteristic distribution of glycosaminoglycans and proteins on it. Their molecules can also cover the surface of cells in the form of the thinnest films and form an intercellular matrix between neighboring cells. Cell contact properties and immune responses are determined by these membrane components.
Many cells, especially those specialized for absorption (intestinal epithelium), have hair-like outgrowths - microvilli on the outer side. The formed or “brush border” carries enzymes, takes part in the breakdown of substances and transport processes. On the basal side of cells specialized for intensive fluid passage (during osmoregulation), for example, in the epithelium of the renal tubules and Malpighian vessels, the membrane forms multiple invaginations that make up the basal labyrinth. The product of cellular secretion, the basement membrane, often separates the epithelium from the deeper cell layers.
Special membrane structures arise at the points of contact of neighboring cells. There are areas where the membranes are so closely adjacent to each other that there is no room for intercellular substance (tight contact). In other areas, complex contact organelles - desmosomes - appear. They and other contact structures serve for mechanical connection and, most importantly, provide chemical and electrical integration of neighboring cells, facilitating intercellular ion transport due to their low electrical resistance.
The structure of an animal cell
1. Cytoplasm and organelles, their function.
2. The nucleus, its structure and functions.
3. Types of division, phases of the cell cycle.
1. The cytoplasm, separated from the environment by the plasmolemma, includes the hyaloplasm, the obligatory cellular components - organelles, as well as various non-permanent structures - inclusions (Fig. 1).
Hyaloplasm (hyalinos - transparent) - the main plasma, or cytoplasmic matrix, is a very important part of the cell, its true internal environment.
In an electron microscope, the matrix looks like a homogeneous and fine-grained substance with a low electron density. Hyaloplasm is a complex colloidal system that includes various biopolymers: proteins, nucleic acids, polysaccharides, etc. This system is able to change from a sol-like (liquid) state to a gel-like state and vice versa. The composition of the hyaloplasm consists mainly of various globular proteins. They make up 20-25% of the total protein content in a eukaryotic cell. The most important enzymes of hyaloplasm include enzymes for the metabolism of sugars, nitrogenous bases, amino acids, lipids and other important compounds. In the hyaloplasm are enzymes for the activation of amino acids in the synthesis of proteins, transport RNA (tRNA). In the hyaloplasm, with the participation of ribosomes and polyribosomes, the synthesis of proteins necessary for proper cellular needs, to maintain and ensure the life of this cell, takes place.
Organelles are microstructures that are constantly present and obligatory for all cells, performing vital functions.
There are membrane organelles - mitochondria, the endoplasmic reticulum (granular and smooth), the Golgi apparatus, lysosomes, and the plasmolemma also belongs to the category of membrane organelles; non-membrane organelles: free ribosomes and polysomes, microtubules, centrioles and filaments (microfilaments). In many cells, organelles can take part in the formation of special structures characteristic of specialized cells. So, cilia and flagella are formed due to centrioles and the plasma membrane, microvilli are outgrowths of the plasma membrane with hyaloplasm and microfilaments, sperm acrosome is a derivative of the elements of the Golgi apparatus, etc.
Fig 1. Ultramicroscopic structure of the cell of animal organisms (scheme)
1 - core; 2 - plasmalemma; 3 - microvilli; 4 - agranular endoplasmic reticulum; 5 - granular endoplasmic reticulum; 6 - Golgi apparatus; 7 - centriole and microtubules of the cell center; 8 - mitochondria; 9 - cytoplasmic vesicles; 10 - lysosomes; 11 - microfilaments; 12 - ribosomes; 13 - isolation of secretion granules.
Membrane organelles are single or interconnected compartments of the cytoplasm, delimited by a membrane from the surrounding hyaloplasm, having their own content, different in composition, properties and functions:
Mitochondria are the organelles for ATP synthesis. Their main function is associated with the oxidation of organic compounds and the use of the energy released during the decay of these compounds for the synthesis of ATP molecules. Mitochondria are also called the energy stations of the cell, or the organelles of cellular respiration.
The term “mitochondria” was introduced by Benda in 1897. Mitochondria can be observed in living cells, because they have a fairly high density. In living cells, mitochondria can move, merge with each other, and divide. The shape and size of the mitochondria of animal cells are varied, but on average their thickness is about 0.5 microns, and their length is from 1 to 10 microns. Their number in cells varies greatly - from single elements to hundreds. So, in the liver cell, they make up more than 20% of the total volume of the cytoplasm. The surface area of all mitochondria of the liver cell is 4-5 times larger than the surface of its plasma membrane.
Mitochondria are bounded by two membranes about 7 nm thick. The outer mitochondrial membrane limits the actual internal contents of the mitochondrion, its matrix. characteristic feature internal membranes of mitochondria is their ability to form numerous protrusions inside the mitochondria. Such invaginations often look like flat ridges, or cristae. Mitochondrial matrix strands are DNA molecules, and small granules are mitochondrial ribosomes.
The endoplasmic reticulum was discovered by K.R. Porter in 1945. This organelle is a collection of vacuoles, flat membrane sacs or tubular formations that create, as it were, a membrane network inside the cytoplasm. There are two types - granular and smooth endoplasmic reticulum.
The granular endoplasmic reticulum is represented by closed membranes, the distinguishing feature of which is that they are covered with ribosomes from the side of the hyaloplasm. Ribosomes are involved in the synthesis of proteins derived from a given cell. In addition, the granular endoplasmic reticulum is involved in the synthesis of enzyme proteins necessary for the organization of intracellular metabolism, and also used for intracellular digestion.
Proteins accumulating in the cavities of the network can, bypassing the hyaloplasm, be transported to the vacuoles of the Golgi complex, where they are often modified and are part of either lysosomes or secretory granules.
The role of the granular endoplasmic reticulum lies in the synthesis of exported proteins on its polysomes, in their isolation from the contents of the hyaloplasm inside the membrane cavities, in the transport of these proteins to other parts of the cell, and in the synthesis of the structural components of cell membranes.
The agranular (smooth) endoplasmic reticulum is also represented by membranes that form small vacuoles and tubes, tubules that can branch with each other. Unlike the granular ER, there are no ribosomes on the membranes of the smooth ER. The diameter of vacuoles and tubules is usually about 50-100 nm.
The smooth endoplasmic reticulum arises and develops at the expense of the granular endoplasmic reticulum.
The activity of smooth EPS is associated with the metabolism of lipids and some intracellular polysaccharides. Smooth ER is involved in the final stages of lipid synthesis. It is highly developed in steroid-secreting cells in the adrenal cortex and in the testis sustentocytes (Sertoli cells).
In striated muscle fibers, smooth ER is able to deposit calcium ions necessary for the function of muscle tissue.
The role of smooth EPS in the deactivation of various substances harmful to the body is very important.
Golgi complex (CG). In 1898, K. Golgi, using the properties of binding heavy metals to cellular structures, revealed mesh formations in nerve cells, which he called the internal mesh apparatus.
It is represented by membrane structures gathered together in a small zone. A separate zone of accumulation of these membranes is called a dictyosome. There can be several such zones in a cell. In the dictyosome, 5-10 flat cisterns are located close to each other (at a distance of 20-25 nm), between which there are thin layers of hyaloplasm. In addition to cisterns, many small vesicles (vesicles) are observed in the CG zone. CG is involved in the segregation and accumulation of products synthesized in the cytoplasmic reticulum, in their chemical rearrangements, maturation; in the cisterns of CG, the synthesis of polysaccharides takes place, their complexation with proteins and, most importantly, the removal of ready-made secrets outside the cell.
Lysosomes are a diverse class of globular structures 0.2-0.4 µm in size, bounded by a single membrane.
A characteristic feature of lysosomes is the presence in them of hydrolytic enzymes that break down various biopolymers. Lysosomes were discovered in 1949 by de Duve.
Peroxisomes are small 0.3-1.5 µm oval-shaped bodies bounded by a membrane. They are especially characteristic of liver and kidney cells. Amino acid oxidation enzymes form hydrogen peroxide, which is destroyed by the enzyme catalase. Peroxisome catalase plays an important protective role, since H2O2 is a toxic substance for the cell.
Non-membrane organelles
Ribosomes - the elementary apparatus for the synthesis of protein, polypeptide molecules - are found in all cells. Ribosomes are complex ribonucleoproteins, which include proteins and RNA molecules. The size of the functioning ribosome of eukaryotic cells is 25 x 20 x 20 nm.
There are single ribosomes and complex ribosomes (polysomes). Ribosomes can be located freely in the hyaloplasm and be associated with the membranes of the endoplasmic reticulum. Free ribosomes form proteins mainly for the cell's own needs, bound provide the synthesis of proteins "for export".
Microtubules are fibrillar components of a protein nature. In the cytoplasm, they can form temporary formations (spindle). Microtubules are part of the centrioles, and are also the main structural elements of cilia and flagella. They are straight, unbranched long hollow cylinders. Their outer diameter is about 24 nm, the inner lumen is 15 nm, and the mesh thickness is 5 nm. Microtubules contain proteins called tubulins. By creating an intracellular skeleton, microtubules can be factors in the oriented movement of the cell as a whole and its intracellular components, creating factors in directed flows of various substances.
Centrioles. The term was proposed by T. Boveri in 1895 to refer to very small bodies. Centrioles usually arranged in a pair - diplosome, are surrounded by a zone of lighter cytoplasm, from which radially thin fibrils (centrosphere) extend. The combination of centrioles and centrosphere is called the cell center. These organelles in dividing cells take part in the formation of the division spindle and are located at its poles. In non-dividing cells, they are located near the CG.
The basis of the structure of centrioles are 9 triplets of microtubules located around the circumference, thus forming a hollow cylinder. Its width is about 0.2 microns, and its length is 0.3-0.5 microns.
In addition to microtubules, centrioles include additional structures - “handles” connecting triplets. Centriole microtubule systems can be described by the formula: (9 x 3) + 0, emphasizing the absence of microtubules in its central part.
In preparing cells for mitotic division, doubling of centrioles occurs.
It is believed that centrioles are involved in the induction of polymerization by tubulin during the formation of microtubules. Before mitosis, the centriole is one of the centers of polymerization of spindle microtubules of cell division.
Cilia and flagella. These are special organelles of movement. At the base of the cilia and flagellum in the cytoplasm, small granules are visible - basal bodies. The length of the cilia is 5-10 microns, the flagella are up to 150 microns.
The cilium is a thin cylindrical outgrowth of the cytoplasm with a diameter of 200 nm. It is covered with a plasma membrane. Inside is an axoneme (“axial thread”), consisting of microtubules.
The axoneme contains 9 doublets of microtubules. Here the system of microtubules is covered with cilia (9 x 2) + 2.
Free cells with cilia and flagella have the ability to move. The way they move is “sliding threads”.
The fibrillar components of the cytoplasm include microfilaments with a thickness of 5-7 nm and the so-called intermediate filaments, microfibrils, with a thickness of about 10 nm.
Microfilaments are found in all cell types. In structure and function, they are different, but it is difficult to distinguish them morphologically from each other. Their chemical composition is different. They can perform the functions of the cytoskeleton and participate in providing movement within the cell.
Intermediate filaments are also protein structures. In the epithelium, they include keratin. Bundles of filaments form tonofibrils that fit into desmosomes. The role of intermediate microfilaments is most likely a support-framework.
inclusions in the cytoplasm. These are optional components of the cell, arising and disappearing depending on the metabolic state of the cells. There are trophic, secretory, excretory and pigment inclusions. Trophic inclusions are neutral fats and glycogen. Pigment inclusions can be exogenous (carotene, dyes, dust particles, etc.) and endogenous (hemoglobin, melanin, etc.). Their presence in the cytoplasm can change the color of the tissue. Often tissue pigmentation serves as a diagnostic sign.
The nucleus provides two groups of general functions: one related to the actual storage and transmission of genetic information, the other - with its implementation, with the provision of protein synthesis.
Reproduction or reduplication of DNA molecules occurs in the nucleus, which makes it possible for two daughter cells during mitosis to obtain exactly the same qualitatively and quantitatively the amount of genetic information.
Another group of cellular processes provided by the activity of the nucleus is the creation of its own apparatus for protein synthesis. This is not only the synthesis, transcription on DNA molecules of various messenger RNAs, but also the transcription of all types of transport and ribosomal RNAs.
Thus, the nucleus is not only a receptacle for genetic material, but also a place where this material functions and reproduces.
The nucleus of a nondividing, interphase cell is usually one per cell. The nucleus consists of chromatin, nucleolus, karyoplasm (nucleoplasm) and a nuclear envelope that separates it from the cytoplasm (karyolemma).
Karyoplasm or nuclear juice is a microscopically structureless substance of the nucleus. It contains various proteins (nucleoproteins, glycoproteins), enzymes and compounds involved in the synthesis of nucleic acids, proteins, and other substances that make up the karyoplasm. Electron - microscopically in the nuclear juice reveal ribonucleoprotein granules 15 nm in diameter.
Glycolytic enzymes involved in the synthesis and cleavage of free nucleotides and their components, enzymes of protein and amino acid metabolism were also found in the nuclear juice. The complex life processes of the nucleus are provided with energy released in the process of glycolysis, the enzymes of which are contained in the nuclear juice.
Chromatin. Chromatin contains DNA in combination with protein. Chromosomes, which are clearly visible during mitotic cell division, have the same properties. The chromatin of the interphase nuclei is a chromosome that loses its compact shape at this time, loosens, decondenses. Zones of complete decondensation are called euchromatin; incomplete loosening of chromosomes - heterochromatin. Chromatin is maximally condensed during mitotic cell division, when it is found in the form of dense chromosomes.
Nucleus. This is one or more rounded bodies 1-5 microns in size, strongly refracting light. It is also called the nucleolus. The nucleolus - the densest structure of the nucleus - is a derivative of the chromosome.
It is now known that the nucleolus is the site of formation of ribosomal RNA and polypeptide chains in the cytoplasm.
The nucleolus is heterogeneous in its structure: in a light microscope one can see its fine-fibrous organization. In an electron microscope, two main components are distinguished: granular and fibrillar. The fibrillar component is the ribonucleoprotein strands of ribosome precursors, the granules are maturing subunits of ribosomes.
The nuclear envelope consists of the outer nuclear membrane and the inner membrane of the envelope, separated by the perinuclear space. The nuclear envelope contains nuclear pores. The membranes of the nuclear membrane do not differ morphologically from other intracellular membranes.
The pores have a diameter of about 80-90 nm. There is a diaphragm across the pore. The pore sizes of this cell are usually stable. The number of pores depends on the metabolic activity of the cells: the more intense the synthetic processes in the cells, the more pores per unit surface of the cell nucleus.
Chromosomes. Both interphase and mitotic chromosomes consist of elementary chromosomal fibrils - DNA molecules.
The morphology of mitotic chromosomes is best studied at the moment of their greatest condensation, in metaphase and at the beginning of anaphase. Chromosomes in this state are rod-shaped structures of varying length and fairly constant thickness. In most chromosomes, it is easy to find the primary constriction zone (centromere), which divides the chromosome into two arms. Chromosomes with equal or almost equal arms are called metacentric, those with arms of unequal length are called submetacentric. Rod-shaped chromosomes with a very short, almost imperceptible second arm are called acrocentric. The kinetochore is located in the region of the primary constriction. Microtubules of the cell spindle emerge from this zone during mitosis. Some chromosomes also have secondary constrictions located near one of the ends of the chromosome and separating a small area - a satellite of the chromosomes. In these places, the DNA responsible for the synthesis of ribosomal RNA is localized.
The totality of the number, size and structural features of chromosomes is called the karyotype of a given species. The karyotype of cattle is 60, horses - 66, pigs - 40, sheep - 54, humans - 46.
The time of existence of a cell as such, from division to division or from division to death, is called the cell cycle (Fig. 2).
The entire cell cycle consists of 4 periods of time: mitosis proper, presynthetic, synthetic, and postsynthetic periods of interphase. During the G1 period, cell growth begins due to the accumulation of cellular proteins, which is determined by an increase in the amount of RNA per cell. In the S - period, the amount of DNA per nucleus doubles and, accordingly, the number of chromosomes doubles. Here, the level of RNA synthesis increases in accordance with the increase in the amount of DNA, reaching its maximum in the G2 period. In the G2 period, the messenger RNA is synthesized, which is necessary for the passage of mitosis. Among the proteins synthesized at this time, a special place is occupied by tubulins - proteins of the mitotic spindle.

Rice. 2. Cell life cycle:
M - mitosis; G1 - pre-synthetic period; S - synthetic period; G2 - postsynthetic period; 1 - old cell (2n4c); 2- young cells (2n2c)
The continuity of the chromosome set is ensured by cell division, which is called mitosis. During this process, a complete rebuild of the kernel takes place. Mitosis consists of a successive series of stages, alternating in a certain order: prophase, metaphase, anaphase and telophase. During mitosis, the nucleus of a somatic cell divides in such a way that each of the two daughter cells receives exactly the same set of chromosomes as the mother cell had.
The ability of cells to reproduce - the most important property living matter. Thanks to this ability, continuous continuity of cellular generations is ensured, the preservation of cellular organization in the evolution of the living, growth and regeneration takes place.
For various reasons (violation of the fission spindle, nondisjunction of chromatids, etc.), cells with large nuclei or multinucleated cells are found in many organs and tissues. This is the result of somatic polyploidy. This phenomenon is called endoreproduction. Polyploidy is more common in invertebrates. In some of them, the phenomenon of polythenia is also common - the construction of a chromosome from many DNA molecules.
Polyploid and polytene cells do not enter mitosis and can divide only by amitosis. The meaning of this phenomenon is that both polyploidy - an increase in the number of chromosomes, and polythenia - an increase in the number of DNA molecules in a chromosome lead to a significant increase in the functional activity of the cell.
In addition to mitosis, science knows two more types of division - amitosis (and - without, mitosis - threads) or direct division and meiosis, which is a process of reducing the number of chromosomes by half by two cell divisions - the first and second division of meiosis (meiosis - reduction). Meiosis is characteristic of germ cells.
Gametogenesis, stages of early embryogenesis
1. The structure of germ cells of vertebrates.
2. Spermatogenesis and ovogenesis.
3. Stages of early embryogenesis.
1. Embryology - the science of the development of the embryo. It studies the individual development of animals from the moment of conception (fertilization of the egg) until its hatching or birth. Embryology considers the development and structure of germ cells and the main stages of embryogenesis: fertilization, cleavage, gastrulation, laying of axial organs and organogenesis, development of provisional (temporary) organs.
The achievements of modern embryology are widely used in animal husbandry, poultry farming, and fish breeding; in veterinary medicine and medicine in solving many practical problems related to artificial insemination and insemination, technology of accelerated reproduction and selection; increasing the fertility of agricultural animals, breeding animals by embryo transplantation, studying the pathology of pregnancy, recognizing the causes of infertility and other obstetric issues.
In structure, sex cells are similar to somatic cells. They also consist of a nucleus and cytoplasm built from organelles and inclusions.
Distinctive properties of mature gametocytes are the low level of assimilation and dissimilation processes, the inability to divide, the content in the nuclei of the haploid (half) number of chromosomes.
Sex cells of males (sperms) in all vertebrates have a flagellar shape (Fig. 3). They are formed in the testes in large quantities. One portion of the isolated semen (ejaculate) contains tens of millions and even billions of sperm.
Sperm of agricultural animals have mobility. Both the size and shape of sperm cells vary greatly from animal to animal. They consist of a head, neck and tail. Sperms are heterogeneous because their nuclei contain different types of sex chromosomes. Half of the spermatozoa have an X chromosome and the other half have a Y chromosome. The sex chromosomes carry the genetic information that determines the sex characteristics of the male. They differ from other chromosomes (autosomes) in their high content of heterochromatin, size and structure.
Sperm have a minimal supply of nutrients, which are very quickly consumed when the cell moves. If the sperm does not merge with the egg, then it usually dies in the female genital tract after 24-36 hours.
You can prolong the life of sperm by freezing. Quinine, alcohol, nicotine and other drugs have a detrimental effect on sperm.
The structure of the egg. The egg is much larger than the sperm. The diameter of oocytes varies from 100 µm to several mm. Vertebrate eggs are oval in shape, immobile, and consist of a nucleus and cytoplasm (Fig. 4). The nucleus contains a haploid set of chromosomes. Mammalian eggs are classified as homogametic, since their nucleus contains only the X chromosome. The cytoplasm contains free ribosomes, endoplasmic reticulum, Golgi complex, mitochondria, yolk and other components. Oocytes are polar. In this connection, two poles are distinguished in them: apical and basal. The peripheral layer of the cytoplasm of the egg is called the cortical layer (cortex - bark). It is completely devoid of yolk, contains many mitochondria.
The eggs are covered with membranes. There are primary, secondary and tertiary membranes. The primary shell is the plasmalemma. The secondary membrane (transparent or shiny) is a derivative of the follicular cells of the ovary. Tertiary membranes are formed in the oviduct in birds: protein, shell and shell membranes of the egg. By the amount of yolk, eggs are distinguished with a small amount - oligolecithal (oligos - few, lecytos - yolk), with an average amount - mesolecithal (mesos - medium) and with a large number - polylecital (poli - a lot).
According to the location of the yolk in the cytoplasm, eggs are distinguished with a uniform distribution of the yolk - isolecithal, or homolecital, and with the localization of the yolk at one pole - telolecital (telos - edge, end). Oligolecithal and isolecithal eggs - in the lancelet and mammals, mesolecithal and telolecithal - in amphibians, some fish, polylecithal and telolecithal - in many fish, reptiles, birds.
2. The ancestors of germ cells are the primary germ cells - gametoblasts (gonoblasts). They are found in the wall of the yolk sac near the blood vessels. Gonoblasts intensively divide by mitosis and migrate with the blood flow or along the course of the blood vessels to the rudiments of the gonads, where they are surrounded by supporting (follicular) cells. The latter perform a trophic function. Then, in connection with the development of the sex of the animal, germ cells acquire properties characteristic of sperm and eggs.
The development of sperm (spermatogenesis) occurs in the testes of a sexually mature animal. There are 4 periods in spermatogenesis: reproduction, growth, maturation and formation.
breeding period. The cells are called spermatogonia. They are small and have a diploid number of chromosomes. Cells rapidly divide by mitosis. The dividing cells are stem cells and replenish the supply of spermatogonia.
Growth period. The cells are called primary spermatocytes. They have a diploid number of chromosomes. The size of the cell increases and complex changes occur in the redistribution of hereditary material in the nucleus, in connection with which four stages are distinguished: leptotenous, zygotenous, pachytic, diplotenous
Ripening period. This is the development of spermatids with half the number of chromosomes.
In the process of maturation, 4 spermatids with a single number of chromosomes arise from each primary spermatocyte. They have well developed mitochondria, Golgi complex, centrosome, located near the nucleus. Other organelles, as well as inclusions, are almost absent. Spermatids are unable to divide.
Formation period. The spermatid acquires morphological properties characteristic of sperm. The Golgi complex is transformed into an acrosome, which encloses the nucleus of the spermatid in the form of a cap. The acrosome is rich in the enzyme hyaluronidase. The centrosome moves to the opposite pole from the nucleus, in which proximal and distal centrioles are distinguished. The proximal centriole remains in the neck of the sperm, while the distal centriole goes to build the tail.
The development of eggs, ovogenesis is a complex and very long process. It begins during the period of embryogenesis and ends in the organs of the reproductive system of a sexually mature female. Oogenesis is composed of three periods: reproduction, growth, maturation.
The reproduction period takes place during the period of intrauterine development and ends within the first months after birth. The cells are called ovogonia and have a diploid number of chromosomes.
During growth, the cells are called primary oocytes. Changes in nuclei are similar to primary spermatocytes. Then, intensive synthesis and accumulation of yolk begins in the oocyte: the stage of previtellogenesis and the stage of vitellogenesis. The secondary membrane of the oocyte consists of a single layer of follicular cells. Previtellogenesis usually lasts until the female reaches puberty. The maturation period consists of rapidly successive maturation divisions during which a diploid cell becomes haploid. This process usually takes place in the oviduct after ovulation.
The first division of maturation ends with the formation of two unequal structures - the secondary oocyte and the first directional or reduction body. During the second division, one mature egg and a second directional body are also formed. The first body is also divided. Consequently, only one mature ovum arises from one primary oocyte in the process of maturation, and the three directional bodies of the latter soon die.
All eggs are genetically homogeneous, since they have only the X chromosome.
3. Fertilization - the fusion of sex gametes and the formation of a new unicellular organism (zygote). It differs from a mature egg cell by a double mass of DNA, a diploid number of chromosomes. Fertilization in mammals is internal, it occurs in the oviduct with its passive movement towards the uterus. The movement of spermatozoa in the female genital tract is carried out due to the function of the movement apparatus of this cell (chemotaxis and rheotaxis), peristaltic contractions of the uterine wall, and the movement of cilia covering the inner surface of the oviduct. When germ cells approach each other, the enzymes of the acrosome of the sperm head destroy the layer of follicular cells, the secondary membrane of the egg. At the moment the sperm touches the plasmolemma of the egg, a protrusion of the cytoplasm is formed on its surface - the fertilization tubercle. The head and neck penetrate into the oocyte. In mammals, only one sperm is involved in fertilization - therefore, the process is called monospermy: XY - male, XX - female.
Birds and reptiles have polyspermy. In birds, all sperm have a Z-chromosome, and eggs have a Z or W-chromosome.
After the penetration of the sperm into the egg, a fertilization membrane is formed around the latter, preventing the penetration of other sperm into the oocyte, the nuclei of germ cells are called: male pronucleus, female pronucleus. The process of their connection is called synkaryon. The centriole introduced by the sperm divides and diverges, forming an achromatin spindle. Crushing begins. Cleavage is a further process of development of a unicellular zygote, during which a multicellular blastula is formed, which consists of a wall - the blastoderm and a cavity - the blastocoel. In the process of mitotic division of the zygote, new cells are formed - blastomeres.
The nature of fragmentation in chordates is different and is largely determined by the type of egg. Cleavage can be complete (holoblastic) or partial (meroblastic). In the first type, all the material of the zygote takes part, in the second - only that zone of it that is devoid of yolk.
Complete crushing is classified into uniform and uneven. The first is characteristic of oligo isolecithal eggs (lancelet, roundworm, etc.). In a fertilized egg, two poles are distinguished: the upper - animal and the lower - vegetative. After fertilization, the yolk moves to the vegetative pole.
Cleavage ends with the formation of a blastula, the shape of which resembles a ball filled with liquid. The wall of the ball is formed by blastoderm cells. Thus, with complete uniform cleavage, the material of the entire zygote participates in cleavage, and after each division, the number of cells doubles.
Complete uneven cleavage is characteristic of mesolecithal (average amount of yolk) and telolecithal oocytes. These are amphibians. Their type of blastula is coeloblastula.
Partial, or meroblastic (discoidal) cleavage is common in fish, birds, and is characteristic of polylecital and telolecital eggs (the type of blastula is called discoblastula).
Gastrulation. With further development of the blastula, in the process of cell division, growth, differentiation and their movements, first a two- and then a three-layer embryo is formed. Its layers are ectoderm, endoderm and mesoderm.
Types of gastrulation: 1) invagination, 2) epiboly (fouling), 3) immigration (settlement), 4) delamination (stratification).
Bookmark axial organs. From these germ layers, axial organs are formed: the rudiment of the nervous system (neural tube), chord and intestinal tube.
In the process of development of the mesoderm, all vertebrates form a notochord, a segmented mesoderm, or somites (spinal segments), and an unsegmented mesoderm, or splanchnot. The latter consists of two sheets: outer - parietal and inner - visceral. The space between these sheets is called the secondary body cavity.
Three rudiments are distinguished in somites: dermatome, myotome, sclerotome. Nephrogonadotom.
With the differentiation of germ layers, embryonic tissue is formed - mesenchyme. It develops from cells that have migrated mainly from the mesoderm and ectoderm. Mesenchyme is a source of development of connective tissue, smooth muscles, blood vessels and other tissues of the animal body. Cleavage processes in various representatives of chordates are very peculiar and depend on the promorphology of the eggs, especially on the amount and distribution of the yolk. The processes of gastrulation also vary greatly within the Chordata.
Thus, gastrulation in the lancelet is typically invagination, it begins with the invagination of the presumptive endoderm. Following the endoderm, the notochord material invaginates into the blastocoel, and the mesoderm plunges through the lateral and ventral lips of the blastopore. The anterior (or dorsal) lip of the blastopore consists of the material of the future nervous system, and from the inside of the cells of the future notochord. As soon as the endodermal layer comes into contact with the inner side of the ectodermal layer, processes begin that lead to the formation of the primordia of axial organs.
The process of gastrulation in bony fish begins when the multilayer blastodisc covers only a small part of the egg yolk, and ends with the complete fouling of the entire “yolk ball”. This means that gastrulation also includes the growth of the blastodisc.
The cellular material of all three germ layers along the anterior and lateral edges of the blastodisc begin to grow onto the yolk. Thus, the so-called yolk sac is formed.
The yolk sac, as part of the embryo, performs a variety of functions:
1) it is an organ with a trophic function, since the differentiating endodermal layer produces enzymes that help break down the substances of the yolk, and blood vessels are formed in the differentiating mesodermal layer, which are in connection with the vascular system of the embryo itself.
2) the yolk sac is a respiratory organ. Gas exchange of the embryo with the external environment occurs through the walls of the vessels of the sac and the ectodermal epithelium.
3) “blood mesenchyme” is the cellular basis of hematopoiesis. The yolk sac is the first hematopoietic organ of the embryo.
Frogs, newts and sea urchins are the main objects of experimental embryological research in the twentieth century.
Invagination in amphibians cannot occur in the same way as in the lancelet, because the vegetative hemisphere of the egg is very overloaded with yolk.
The first noticeable sign of incipient gastrulation in frogs is the appearance of a blastopore, i.e., an indentation or gap in the middle of the gray crescent.
The behavior of the cellular material of the nervous system and the epidermis of the skin deserves special attention. In the end, the future epidermis and material of the nervous system covers the entire surface of the embryo. The presumptive epidermis of the skin moves and thins in all directions. The set of cells of the presumptive nervous system moves almost exclusively in meridional directions. The layer of cells of the future nervous system in the transverse direction is reduced, the presumptive region of the nervous system is elongated in the animal-vegetative direction.
Let us summarize what we know about the fate of each of the germ layers.
Ectoderm derivatives. From the cells that make up the outer layer, multiplying and differentiating, they form: the outer epithelium, skin glands, the surface layer of teeth, horny scales, etc. By the way, almost always every organ develops from the cellular elements of two, or even all three germ layers . For example, mammalian skin develops from ectoderm and mesoderm.
An extensive part of the primary ectoderm "plunges" inward, under the outer epithelium, and gives rise to the entire nervous system.
Endoderm derivatives. The internal germ layer develops into the epithelium of the midgut and its digestive glands. The epithelium of the respiratory system develops from the anterior intestine. But the cellular material of the so-called prechordal plate is involved in its origin.
derivatives of the mesoderm. All muscle tissues, all types of connective, cartilaginous, bone tissues, channels of the excretory organs, the peritoneum of the body cavity, the circulatory system, part of the tissues of the ovaries and testes develop from it.
In most animals, the middle layer appears not only in the form of a collection of cells that form a compact epithelial layer, that is, the mesoderm proper, but in the form of a loose complex of scattered, amoeba-like cells. This part of the mesoderm is called the mesenchyme. Actually, the mesoderm and mesenchyme differ from each other in their origin, there is no direct connection between them, they are not homologous. The mesenchyme is mostly of ectodermal origin, while the mesoderm originates from the endoderm. In vertebrates, however, the mesenchyme shares a common origin with the rest of the mesoderm.
In all animals that tend to have a coelom (secondary body cavity), the mesoderm gives rise to hollow coelomic sacs. Coelomic sacs form symmetrically on the sides of the intestine. The wall of each coelomic sac facing the intestine is called the splanchnopleura. The wall facing the ectoderm of the embryo is called the somatopleura.
Thus, during the development of the embryo, various cavities are formed that have important morphogenetic significance. First, Baer's cavity appears, turning into the primary body cavity - the blastocoel, then the gastrocoel (or gastric cavity) appears, and finally, in many animals, the whole. With the formation of the gastrocoel and coelom, the blastocoel decreases more and more, so that only gaps in the gaps between the walls of the intestine and the coelom remain from the former primary body cavity. These gaps turn into cavities of the circulatory system. The gastrocoel eventually transforms into the cavity of the midgut.
Features of the embryogenesis of mammals and birds
1. Extra-embryonic organs.
2. Mammalian placenta.
3. Stages of the prenatal ontogenesis of ruminants, pigs and birds.
1. In embryos of reptiles and birds, a yolk sac is also formed. All germ layers are involved in this. During the 2nd and 3rd days of development of the chicken embryo, a network of blood vessels develops in the inner part of the area opaca. Their appearance is inextricably linked with the emergence of embryonic hematopoiesis. Thus, one of the functions of the yolk sac of avian embryos is embryonic hematopoiesis. In the embryo itself, only subsequently, hematopoietic organs are formed - the liver, spleen, bone marrow.
The heart of the fetus begins to function (contract) at the end of the second day, from that time there is blood flow.
In bird embryos, in addition to the yolk sac, three more provisional organs are formed, which are commonly called embryonic membranes - amnion, serosa and allantois. These organs can be considered as developed in the process of evolutionary adaptation of embryos.
Amnion and serosa arise in the closest relationship. Amnion in the form of a transverse fold, growing, bends over the anterior end of the head of the embryo and covers it like a hood. In the future, the lateral sections of the amniotic folds grow on both sides of the embryo itself and grow together. The amniotic folds are composed of ectoderm and parietal mesoderm.
In conjunction with the wall of the amniotic cavity, another important provisional formation develops - the serosa, or serous membrane. It consists of an ectodermal leaf, “looking” at the embryo, and a mesodermal, “looking” outward. The outer shell grows over the entire surface under the shell. This is serosa.
Amnion and serosa are, of course, "shells", because they really cover and unite the embryo itself from the external environment. However, these are organs, parts of the embryo with very important functions. Amniotic fluid creates aquatic environment for animal embryos that have become terrestrial in the course of evolution. It protects the developing embryo from drying out, from shaking, from sticking to the egg shell. It is interesting to note that the role of amniotic fluid in mammals was noted by Leonardo da Vinci.
The serous membrane takes part in respiration and resorption of the remnants of the protein membrane (under the action of enzymes secreted by the chorion).
Another provisional organ develops - allantois, which first performs the function of the embryonic bladder. It appears as a ventral outgrowth of the hindgut endoderm. In a chicken embryo, this protrusion appears already on the 3rd day of development. In the middle of the embryonic development of birds, allantois grows under the chorion over the entire surface of the embryo with the yolk sac.
At the very end of the embryonic development of birds (and reptiles), the provisional organs of the embryo gradually stop their functions, they are reduced, the embryo begins to breathe the air inside the egg (in the air chamber), breaks through the shell, is released from the egg membranes and finds itself in the external environment.
The extra-embryonic organs of mammals are the yolk sac, amnion, allantois, chorion and placenta (Fig. 5).
2. In mammals, the connection of the embryo with the mother's body is ensured by the formation of a special organ - the placenta (children's place). The source of its development is the allanto-chorion. Placentas are divided into several types according to their structure. The classification is based on two principles: a) the nature of the distribution of chorionic villi and 2) the way they are connected with the uterine mucosa (Fig. 6).
The shape distinguishes several types of placenta:
1) Diffuse placenta (epitheliochorial) - its secondary papillae develop over the entire surface of the chorion. The chorionic villi penetrate the glands of the uterine wall without destroying the uterine tissue. The nutrition of the embryo is carried out through the uterine glands, which secrete royal jelly, which is absorbed into the blood vessels of the chorionic villi. During childbirth, the chorionic villi are pushed out of the uterine glands without tissue destruction. Such a placenta is typical for pigs, horses, camels, marsupials, cetaceans, hippopotamus.

Rice. 5. Scheme of development of the yolk sac and embryonic membranes in mammals (six successive stages):
A - the process of fouling of the cavity of the fetal bladder with endoderm (1) and mesoderm (2); B - formation of a closed endodermal vesicle (4); B - the beginning of the formation of the amniotic fold (5) and the intestinal groove (6); G - isolation of the body of the embryo (7); yolk sac (8); D - closure of amniotic folds (9); the beginning of the formation of the development of allantois (10); E - closed amniotic cavity (11); developed allantois (12); chorionic villi (13); parietal sheet of mesoderm (14); visceral sheet of mesoderm (15); ectoderm (3).
2) Cotyledon placenta (desmochorionic) - chorionic villi are located in bushes - cotyledons. They connect with thickenings of the uterine wall, which are called caruncles. The cotyledon-caruncle complex is called the placenta. Such a placenta is characteristic of ruminants.
3) Girdle placenta (endotheliochorionic) - villi in the form of a wide belt surround the fetal bladder and are located in the connective tissue layer of the uterine wall, in contact with the endothelial layer of the wall of blood vessels.
4) Discoidal placenta (hemochorial) - the contact zone of the chorionic villi and the wall of the uterus has the shape of a disk. The chorionic villi sink into blood-filled lacunae lying in the connective tissue layer of the uterine wall. This placenta is found in primates.
3. Livestock workers, through their practical activities, breed and raise animals. These are complex biological processes, and in order to consciously manage or seek ways to improve them, the zoo engineer and veterinarian must know the basic patterns of animal development throughout their individual lives. We already know that the chain of changes that an organism goes through from its inception to natural death is called ontogeny. It is composed of qualitatively different periods. However, the periodization of ontogeny has not yet been sufficiently developed. Some scientists believe that the ontogenetic development of an organism begins with the development of germ cells, others - with the formation of a zygote.

Rice. 6. Types of histological structure of placenta:
A - epitheliochorial; B - desmochorial; C - endotheliochorial; G - hemochorial; I - germinal part; II - maternal part; 1 - epithelium: 2 - connective tissue and 3 - endothelium of the blood vessel of the chorionic villus; 4 - epithelium; 5 - connective tissue and 6 - blood vessels and lacunae of the uterine mucosa.
After the appearance of the zygote, the subsequent ontogeny of agricultural animals is divided into intrauterine and postnatal development.
The duration of sub-periods of intrauterine development of agricultural animals, days (according to G.A. Schmidt).
In the embryogenesis of animals, due to their relationship, there are some fundamentally similar features: 1) the formation of a zygote, 2) crushing, 3) the formation of germ layers, 4) differentiation of germ layers, leading to the formation of tissues and organs.
General histology. epithelial tissues
1. Development of tissues.
2. Classification of epithelial tissues.
3. Glands and criteria for their classification.
1. The animal body is built from cells and non-cellular structures specialized in performing certain functions. Populations of cells, different in function, differ in the structure and specificity of the synthesis of intracellular proteins.
In the process of development, initially homogeneous cells acquired differences in metabolism, structure, and function. This process is called differentiation. In this case, genetic information is realized that comes from the DNA of the cell nucleus, which manifests itself in specific conditions. The adaptation of cells to these conditions is called adaptation.
Differentiation and adaptation determine the development of qualitatively new interrelations and relationships between cells and their populations. At the same time, the importance of the integrity of the organism, i.e., integration, increases to a large extent. So, each stage of embryogenesis is not just an increase in the number of cells, but a new state of integrity.
Integration is the unification of cell populations into more complex functioning systems - tissues, organs. It can be broken by viruses, bacteria, X-rays, hormones and other factors. In these cases biological system out of control, which can cause the development of malignant tumors and other pathologies.
Morphofunctional and genetic differences that arose in the process of phylogenesis allowed cells and non-cellular structures to unite into so-called histological tissues.
A tissue is a historically established system of cells and non-cellular structures, characterized by a common structure, function and origin.
There are four main types of tissues: epithelial, connective or support-trophic, muscle and nervous. There are other classifications as well.
2. Epithelial tissues communicate the body with the external environment. They perform integumentary and glandular (secretory) functions. The epithelium is located in the skin, lines the mucous membranes of all internal organs; it has the functions of absorption, excretion. Most of the body's glands are built from epithelial tissue.
All germ layers take part in the development of epithelial tissue.
All epithelia are built from epithelial cells - epitheliocytes. Connecting firmly to each other with the help of desmosomes, closure bands, gluing bands and by interdigitation, epitheliocytes form a cell layer that functions and regenerates. Typically, the layers are located on the basement membrane, which, in turn, lies on loose connective tissue that feeds the epithelium (Fig. 7).
Epithelial tissues are characterized by polar differentiation, which is reduced to a different structure or layers of the epithelial layer, or poles of epitheliocytes. For example, at the apical pole, the plasmolemma forms an absorptive border or ciliated cilia, while the nucleus and most organelles are located at the basal pole.
Depending on the location and function performed, two types of epithelium are distinguished: integumentary and glandular.
The most common classification of integumentary epithelium is based on the shape of cells and the number of layers in the epithelial layer, therefore it is called morphological.
3. The epithelium that produces secrets is called glandular, and its cells are called secretory cells, or secretory glandulocytes. Glands are built from secretory cells, which can be designed as an independent organ or are only part of it.
Distinguish between endocrine and exocrine glands. Morphologically, there is a difference in the presence of an excretory duct in the latter. Exocrine glands can be unicellular or multicellular. Example: goblet cell in simple columnar border epithelium. By the nature of the branching of the excretory duct, simple and complex are distinguished. Simple glands have a non-branching excretory duct, while complex glands have a branching one. The terminal sections in simple glands branch and unbranch, in complex glands they branch.
According to the shape of the terminal sections, exocrine glands are classified into alveolar, tubular and tubular-alveolar. The cells of the terminal section are called glandulocytes.
According to the method of secretion formation, the glands are divided into holocrine, apocrine and merocrine. These are sebaceous, then sweat and mammary glands of the stomach, respectively.
Regeneration. Integumentary epithelium occupy a border position. They are often damaged, therefore they are characterized by a high regenerative capacity. Regeneration is carried out mainly by the mitotic method. The cells of the epithelial layer quickly wear out, age and die. Their restoration is called physiological regeneration. The restoration of epithelial cells lost due to injury is called reparative regeneration.
In single-layer epithelium, all cells have a regenerative ability, in multi-layered epithelium - stem cells. In the glandular epithelium, with holocrine secretion, stem cells located on the basement membrane have this ability. In the merocrine and apocrine glands, the restoration of epitheliocytes proceeds mainly through intracellular regeneration.

Rice. 7. Scheme of different types of epithelium
A. Single layer flat.
B. Single layer cubic.
B. Single-layer cylindrical.
G. Multi-row cylindrical ciliated.
D. Transitional.
E. Multilayer flat non-keratinized.
G. Multilayer flat keratinizing.
Support-trophic tissues. blood and lymph
1. Blood. Blood cells.
3. Hemocytopoiesis.
4. Embryonic hemocytopoiesis.
With this topic, we begin the study of a group of related tissues, referred to as connective. These include: connective tissue proper, blood cells and hematopoietic tissues, skeletal tissues (cartilaginous and bone), connective tissues with special properties.
The manifestation of the unity of the above types of tissue is their origin from a common embryonic source - the mesenchyme.
Mesenchyme - a set of embryonic network-like process cells that fill the gaps between the germ layers and the rudiments of organs. In the body of the embryo, the mesenchyme arises mainly from the cells of certain sections of the mesoderm - dermatomes, sclerotomes and splanchnotomes. Mesenchymal cells rapidly divide by mitosis. Numerous mesenchymal derivatives arise in its various parts - blood islands with their endothelium and blood cells, cells of connective tissues and smooth muscle tissue, etc.
1. Intravascular blood - a mobile tissue system with a liquid intercellular substance - plasma and formed elements - erythrocytes, leukocytes and platelets.
Constantly circulating in a closed circulatory system, blood unites the work of all body systems and maintains many physiological indicators of the internal environment of the body at a certain level that is optimal for metabolic processes. Blood performs various vital functions in the body: respiratory, trophic, protective, regulatory, excretory, and others.
Despite the mobility and variability of blood, its indicators at every moment correspond to the functional state of the body, so blood testing is one of the most important diagnostic methods.
Plasma - a liquid component of blood, contains 90-92% water and 8-10% solids, including 9% organic and 1% mineral substances. The main organic substances of blood plasma are proteins (albumins, various fractions of globulins and fibrinogen). Immune proteins (antibodies), and most of them are contained in the gamma globulin fraction, are called immunoglobulins. Albumins provide the transfer of various substances - free fatty acids, bilirubin, etc. Fibrinogen takes part in the processes of blood coagulation.
Erythrocytes are the main type of blood cells, since there are 500-1000 times more of them than leukocytes. 1 mm 3 of the blood of cattle contains 5.0-7.5 million, horses - 6-9 million, sheep - 7-12 million, goats - 12-18 million, pigs - 6-7.5 million, chickens - 3-4 million red blood cells.
Having lost the nucleus during development, mature erythrocytes in mammals are nuclear-free cells and have the shape of a biconcave disk with an average circle diameter of 5-7 microns. Camel and llama blood erythrocytes are oval. The disk-shaped form increases the total surface of the erythrocyte by 1.64 times.
There is an inverse relationship between the number of red blood cells and their size.
Erythrocytes are covered with a membrane - plasmolemma (6 nm thick), containing 44% lipids, 47% proteins and 7% carbohydrates. The erythrocyte membrane is easily permeable to gases, anions, and Na ions.
The internal colloidal content of erythrocytes by 34% consists of hemoglobin - a unique complex colored compound - a chromoprotein, in the non-protein part of which (heme) there is ferrous iron, capable of forming special fragile bonds with an oxygen molecule. It is thanks to hemoglobin that the respiratory function of red blood cells is carried out. Oxyhemoglobin \u003d hemoglobin + O2.
The presence of hemoglobin in erythrocytes causes their pronounced oxyphilia when staining a blood smear according to Romanovsky-Giemsa (eosin + azure II). Erythrocytes are stained red with eosin. In some forms of anemia, the central pale colored part of the erythrocytes is enlarged - hypochromic erythrocytes. With supravital blood staining with brilliant cresyl blue, young forms of erythrocytes containing granular-mesh structures can be detected. Such cells are called reticulocytes, they are the immediate precursors of mature erythrocytes. The reticulocyte count is used to obtain information about the rate of formation of red blood cells.
The life span of an erythrocyte is 100-130 days (in rabbits 45-60 days). Erythrocytes have the ability to withstand various destructive influences - osmotic, mechanical, etc. With changes in the concentration of salts in the environment, the erythrocyte membrane ceases to retain hemoglobin, and it enters the surrounding fluid - the phenomenon of hemolysis. The release of hemoglobin can occur in the body under the action of snake venom, toxins. Hemolysis also develops during the transfusion of incompatible blood types. It is practically important when introducing liquids into the blood of animals to control that the injected solution is isotonic.
RBCs have a relatively high density compared to plasma and leukocytes. If the blood is treated with anticoagulants and placed in a vessel, then erythrocyte sedimentation is noted. The erythrocyte sedimentation rate (ESR) in animals of different ages, sex and species is not the same. High ESR in horses and, conversely, low in cattle. ESR has diagnostic and prognostic value.
Leukocytes are vascular blood cells that are diverse in morphological features and functions. In the animal body, they perform a variety of functions aimed primarily at protecting the body from foreign influences through phagocytic activity, participation in the formation of humoral and cellular immunity, as well as in the recovery processes in tissue damage. In 1 mm3 of blood in cattle, there are 4.5-12 thousand of them, in horses - 7-12 thousand, in sheep - 6-14 thousand, in pigs - 8-16 thousand, in chickens - 20-40 thousand. An increase in the number of leukocytes - leukocytosis - is a characteristic feature for many pathological processes.
Formed in the hematopoietic organs and entering the blood, leukocytes only stay in the vascular bed for a short time, then migrate to the surrounding vascular connective tissue and organs, where they perform their main function.
The peculiarity of leukocytes is that they have mobility due to the resulting pseudopodia. In leukocytes, a nucleus and cytoplasm are distinguished, containing various organelles and inclusions. The classification of leukocytes is based on the ability to stain with dyes and granularity.
Granular leukocytes (granulocytes): neutrophils (25-70%), eosinophils (2-12%), basophils (0.5-2%).
Non-granular leukocytes (agranulocytes): lymphocytes (40-65) and monocytes (1-8%).
A certain percentage ratio between individual types of leukocytes is called a leukocyte formula - a leukogram.
An increase in the percentage of neutrophils in the leukogram is typical for purulent-inflammatory processes. In mature neutrophils, the nucleus consists of several segments connected by thin bridges.
On the surface of basophils, there are special receptors that bind immunoglobulins E. They are involved in allergic-type immunological reactions.
Monocytes circulating in the blood are precursors of tissue and organ macrophages. After staying in the vascular blood (12-36 hours), monocytes migrate through the endothelium of capillaries and venules into tissues and turn into mobile macrophages.
Lymphocytes are the most important cells involved in various immunological reactions of the body. A large number of lymphocytes are found in the lymph.
There are two main classes of lymphocytes: T- and B-lymphocytes. The first develop from bone marrow cells in the cortical part of the thymus lobules. In the plasmalemma, they have antigenic markers and numerous receptors, with the help of which foreign antigens and immune complexes are recognized.
B-lymphocytes are formed from stem precursors in the bursa of Fabricius (Bursa). Their place of development is considered myeloid tissue of the bone marrow.
The effector cells in the T-lymphocyte system are three main subpopulations: T-killers (cytotoxic lymphocytes), T-helpers (helpers) and T-suppressors (depressors). The effector cells of B-lymphocytes are plasmablasts and mature plasma cells capable of producing immunoglobulins in an increased amount.
Platelets are non-nuclear elements of the vascular blood of mammals. These are small cytoplasmic fragments of red bone marrow megakaryocytes. In 1 mm3 of their blood, there are 250-350 thousand platelets. In birds, cells that function similarly are called platelets.
Blood platelets have the most important knowledge in providing the main stages of stopping bleeding - hemostasis.
2. Lymph - an almost transparent yellowish liquid located in the cavity of the lymphatic capillaries and vessels. Its formation is due to the transition of the constituent parts of the blood plasma from the blood capillaries into the tissue fluid. In the formation of lymph, the relationship between the hydrostatic and osmotic pressure of blood and tissue fluid, the permeability of the walls of blood capillaries, etc., are essential.
Lymph consists of a liquid part - lymphoplasm and formed elements. Lymphoplasma differs from blood plasma by a lower content of proteins. The lymph contains fibrinogen, so it is also capable of clotting. The main formed elements of lymph are lymphocytes. The composition of lymph in different vessels of the lymphatic system is not the same. There are peripheral lymph (before the lymph nodes), intermediate (after the lymph nodes) and central (lymph of the thoracic and right lymphatic ducts), the richest in cellular elements.
3. Hematopoiesis (hemocytopoiesis) is a multi-stage process of successive cellular transformations leading to the formation of mature peripheral vascular blood cells.
In the postembryonic period in animals, the development of blood cells is carried out in two specialized intensively renewing tissues - myeloid and lymphoid.
Currently, the most recognized is the scheme of hematopoiesis proposed by I.L. Chertkov and A.I. Vorobyov (1981), according to which the entire hemocytopoiesis is divided into 6 stages (Fig. 8).
The ancestor of all blood cells (according to A.A. Maksimov) is a pluripotent stem cell (a colony-forming unit in the spleen and CFUs). In the adult body the largest number stem cells are located in the red bone marrow (about 50 stem cells per 100,000 bone marrow cells), from which they migrate to the thymus, spleen.
The development of erythrocytes (erythrocytopoiesis) in the red bone marrow proceeds according to the scheme: stem cell (SC) - half-stem cells (CFU - GEMM, CFU - GE, CFU - MGCE) - unipotent precursors of erythropoiesis (PFU - E, CFU - E) - erythroblast - pronormocyte - basophilic normocyte - polychromatophilic normocyte - oxyphilic normocyte - reticulocyte - erythrocyte.
Development of granulocytes: stem cell of the red bone marrow, semi-stem (CFU - GEMM, CFU - GM, CFU - GE), unipotent precursors (CFU - B, CFU - Eo, CFU - Gn), which through the stages of recognizable cell forms turn into mature segmented nuclear granulocytes of three varieties - neutrophils, eosinophils and basophils.
The development of lymphocytes is one of the most complex processes of hematopoietic stem cell differentiation.
With the participation of various organs, the formation of two closely related cell lines, T- and B-lymphocytes, is carried out step by step.
The development of platelets occurs in the red bone marrow and is associated with the development of special giant cells in it - megakaryocytes. Megakaryocytopoiesis consists of the following stages: SC - semi-stem cells (CFU - GEMM and CFU - MGCE) - unipotent precursors, (CFU - MHC) - megakaryoblast - promegakaryocyte - megakaryocyte.
4. At the earliest stages of ontogenesis, blood cells are formed outside the embryo, in the mesenchyme of the yolk sac, where clusters are formed - blood islands. The central cells of the islets are rounded and converted into hematopoietic stem cells. The peripheral cells of the islets stretch into strips, interconnected cells and form the endothelial lining of the primary blood vessels (the vasculature of the yolk sac). Part of the stem cells turns into large basophilic blast cells - primary blood cells. Most of these cells, intensively multiplying, are increasingly stained with acidic dyes. This occurs in connection with the synthesis and accumulation of hemoglobin in the cytoplasm, and condensed chromatin in the nucleus. These cells are called primary erythroblasts. In some primary erythroblasts, the nucleus disintegrates and disappears. The resulting generation of nuclear and non-nuclear primary erythrocytes is diverse in size, but the most common are large cells - megaloblasts and megalocytes. The megaloblastic type of hematopoiesis is characteristic of the embryonic period.
Part of the primary blood cells is converted into a population of secondary erythrocytes, and outside the vessels, no a large number of granulocytes - neutrophils and eosinophils, that is, myelopoiesis occurs.
The stem cells that arise in the yolk sac are transported with blood to the organs of the body. After laying the liver, it becomes a universal organ of hematopoiesis (secondary erythrocytes, granular leukocytes and megakaryocytes develop). By the end of the intrauterine period, hematopoiesis in the liver stops.
At 7-8 weeks of embryonic development (in cattle), thymus lymphocytes and T-lymphocytes migrating from it differentiate from stem cells in the developing thymus. The latter inhabit the T-zones of the spleen and lymph nodes. At the beginning of its development, the spleen is also an organ in which all types of blood cells are formed.
At the last stages of embryonic development in animals, the main hematopoietic functions begin to be performed by the red bone marrow; it produces erythrocytes, granulocytes, platelets, part of lymphocytes (V-l). In the postembryonic period, the red bone marrow becomes an organ of universal hematopoiesis.
During embryonic erythrocytopoiesis, there is a characteristic process of changing generations of erythrocytes, which differ in morphology and type of hemoglobin formed. The population of primary erythrocytes forms the embryonic type of hemoglobin (Hb - F). at subsequent stages, erythrocytes in the liver and spleen contain the fetal (fetal) type of hemoglobin (Hb-G). In the red bone marrow, a definitive type of erythrocytes with a third type of hemoglobin (Hb-A and Hb-A 2) are formed. different types hemoglobins differ in the composition of amino acids in the protein part.
cell embryogenesis tissue histology cytology
Connective tissue proper
1. Loose and dense connective tissue.
2. Connective tissue with special properties: reticular, adipose, pigmented.
1. Widespread tissues in the animal body with a highly developed system of fibers in the intercellular substance, thanks to which these tissues perform versatile mechanical and shaping functions - they form a complex of partitions, trabeculae or layers inside organs, are part of numerous membranes, form capsules, ligaments, fascia , tendons.
Depending on the quantitative ratio between the components of the intercellular substance - fibers and the main substance, and in accordance with the type of fibers, three types of connective tissues are distinguished: loose connective tissue, dense connective tissue and reticular tissue.
The main cells that create the substances necessary for building fibers in loose and dense connective tissue are fibroblasts, in reticular tissue - reticular cells. Loose connective tissue is characterized by a particularly large variety of cellular composition.
Loose connective tissue is the most common. It accompanies all blood and lymphatic vessels, forms numerous layers inside organs, etc. It consists of a variety of cells, the main substance and a system of collagen and elastic fibers. In the composition of this tissue, more sedentary cells are distinguished (fibroblasts - fibrocytes, lipocytes), mobile (histiocytes - macrophages, tissue basophils, plasmocytes) - Fig. 9.
The main functions of this connective tissue are trophic, protective and plastic.
Types of cells: Adventitial cells are poorly differentiated, capable of mitotic division and transformation into fibroblasts, myofibroblasts and lipocytes. Fibroblasts are the main cells that are directly involved in the formation of intercellular structures. During embryonic development, fibroblasts arise directly from mesenchymal cells. There are three types of fibroblasts: poorly differentiated (function: synthesis and secretion of glycosaminoglycans); mature (function: synthesis of procollagen, proelastin, enzyme proteins and glycosaminoglycans, especially - protein synthesis of collagen fibers); myofibroblasts that promote wound closure. Fibrocytes lose their ability to divide, reduce their synthetic activity. Histiocytes (macrophages) belong to the system of mononuclear phagocytes (MPS). This system will be discussed in the next lecture. Tissue basophils (labrocytes, mast cells), located near small blood vessels, they are one of the first cells to respond to the penetration of antigens from the blood.
Plasmocides - functionally - effector cells of immunological reactions of the humoral type. These are highly specialized cells of the body that synthesize and secrete the bulk of various antibodies (immunoglobulins).
The intercellular substance of loose connective tissue is a significant part of it. It is represented by collagen and elastic fibers and the main (amorphous) substance.
Amorphous substance - a product of the synthesis of connective tissue cells (mainly fibroblasts) and the intake of substances from the blood, transparent, slightly yellowish, capable of changing its consistency, which significantly affects its properties.
It consists of glycosaminoglycans (polysaccharides), proteoglycans, glycoproteins, water and inorganic salts. The most important chemical high-polymer substance in this complex is a non-sulfated variety of glycosaminoglycans - hyaluronic acid.
Collagen fibers consist of fibrils formed by tropocollagen protein molecules. The latter are peculiar monomers. The formation of fibrils is the result of a characteristic grouping of monomers in the longitudinal and transverse directions.
Depending on the amino acid composition and the form of chains combining into a triple helix, there are four main types of collagen that have different localization in the body. Type I collagen is found in the connective tissue of the skin, tendons, and bones. Collagen type II - in hyaline and fibrous cartilage. Collagen II? type - in the skin of embryos, the wall of blood vessels, ligaments. Collagen type IV - in basement membranes.
There are two ways of forming collagen fibers: intracellular and extracellular synthesis.
Elastic fibers are homogeneous threads that form a network. Do not combine into bundles, have low strength. There is a more transparent amorphous central part, consisting of elastin protein, and a peripheral part, consisting of microfibrils of a glycoprotein nature, shaped like tubules. Elastic fibers are formed due to the synthetic and secretory function of fibroblasts. It is believed that at first, in the immediate vicinity of fibroblasts, a framework of microfibrils is formed, and then the formation of an amorphous part from the precursor of elastin, proelastin, is enhanced. Proelastin molecules under the influence of enzymes shorten and turn into tropoelastin molecules. The latter, during the formation of elastin, are interconnected with the help of desmosine, which is absent in other proteins. Elastic fibers predominate in the occipital-cervical ligament, abdominal yellow fascia.
Dense connective tissue. This tissue is characterized by a quantitative predominance of fibers over the main substance and cells. Depending on the relative position fibers and networks formed from the bottom of the bundles, there are two main types of dense connective tissue: unformed (dermis) and formed (ligaments, tendons).
2. Reticular tissue consists of process reticular cells and reticular fibers (Fig. 10). Reticular tissue forms the stroma of hematopoietic organs, where, in combination with macrophages, it creates a microenvironment that ensures the reproduction, differentiation and migration of various blood cells.
Reticular cells develop from mesenchymocytes and are similar to fibroblasts, chondroblasts, etc. Reticular fibers are derivatives of reticular cells and are thin branching fibers that form a network. They contain fibrils of various diameters, enclosed in an interfibrillar substance. The fibrils are composed of type III collagen.
Adipose tissue is made up of fat cells (lipocytes). The latter are specialized in the synthesis and accumulation of storage lipids in the cytoplasm, mainly triglycerides. Lipocytes are widely distributed in loose connective tissue. In embryogenesis, fat cells arise from mesenchymal cells.
Precursors for the formation of new fat cells in the postembryonic period are the adventitial cells that accompany the blood capillaries.
There are two types of lipocytes and actually two types of adipose tissue: white and brown. White adipose tissue is contained in the body of animals differently depending on the species and breed. There is a lot of it in fat depots. The total amount of it in the body of animals of various species, breeds, sex, age, fatness ranges from 1 to 30% of the fat mass. Fat as an energy source (1 g of fat = 39 kJ), water depot, shock absorber.

Rice. 11. The structure of white adipose tissue (scheme according to Yu.I. Afanasiev)
A - adipocytes with removed fat in a light optical microscope; B - ultramicroscopic structure of adipocytes. 1 - the nucleus of the fat cell; 2 - large drops of lipids; 3 - nerve fibers; 4 - hemocapillaries; 5 - mitochondria.

Rice. 12. The structure of brown adipose tissue (scheme according to Yu.I. Afanasiev)
A - adipocytes with removed fat in a light optical microscope; B - ultramicroscopic structure of adipocytes. 1 - adipocyte nucleus; 2 - finely divided lipids; 3 - numerous mitochondria; 4 - hemocapillaries; 5 - nerve fiber.
Brown adipose tissue is found in significant quantities in rodents and hibernating animals; as well as in newborns of other species. Cells, oxidized, form heat, which goes to thermoregulation.
Pigment cells (pigmentocytes) have many dark brown or black pigment grains from the melanin group in the cytoplasm.
The immune system and cellular interactions in immune responses
1. The concept of antigens and antibodies, their varieties.
2 The concept of cellular and humoral immunity.
3 Genesis and interaction of T- and B-lymphocytes.
4 Mononuclear system of macrophages.
1. In industrial animal husbandry, under conditions of concentration and intensive exploitation of livestock, stressful effects of technogenic and other environmental factors, the role of preventing animal diseases, especially young animals, due to the impact of various agents of infectious and non-infectious nature, against the background of a decrease in the natural protective abilities of the body, increases significantly.
Concerning great importance acquires the problem of controlling the physiological and immunological state of animals in order to timely increase their general and specific resistance (Tsymbal A.M., Konarzhevsky K.E. et al., 1984).
Immunity (immunitatis - liberation from something) is the protection of the body from everything genetically alien - microbes, viruses, from alien cells. or genetically modified own cells.
The immune system combines organs and tissues in which the formation and interaction of cells takes place - immunocytes that perform the function of recognizing genetically alien substances (antigens) and carrying out a specific reaction.
Antibodies are complex proteins found in the immunoglobulin fraction of animal blood plasma, synthesized by plasma cells under the influence of various antigens. Several classes of immunoglobulins (Y, M, A, E, D) have been studied.
At the first encounter with an antigen (primary response), lymphocytes are stimulated and undergo transformation into blast forms that are capable of proliferating and differentiating into immunocytes. Differentiation leads to the appearance of two types of cells - effector and memory cells. The former are directly involved in the elimination of foreign material. Effector cells include activated lymphocytes and plasma cells. Memory cells are lymphocytes that return to an inactive state, but carry information (memory) about a meeting with a specific antigen. With the repeated introduction of this antigen, they are able to provide a rapid immune response (secondary response) due to increased proliferation of lymphocytes and the formation of immunocytes.
2. Depending on the mechanism of antigen destruction, cellular immunity and humoral immunity are distinguished.
In cellular immunity, effector (motor) cells are cytotoxic T-lymphocytes, or killer lymphocytes (killers), which are directly involved in the destruction of foreign cells of other organs or pathological own cells (for example, tumor cells) and secrete lytic substances.
In humoral immunity, the effector cells are plasma cells that synthesize and secrete antibodies into the blood.
In the formation of cellular and humoral immunity in humans and animals, cellular elements of lymphoid tissue, in particular T- and B-lymphocytes, play an important role. Information about the populations of these cells in the blood of cattle is scarce. According to Korchan N.I. (1984), calves are born with a relatively mature B-lymphocyte system and an underdeveloped B-lymphocyte system and regulatory relationships between these cells. Only by the 10-15th day of life, the indicators of these cell systems approach those of adult animals.
The immune system in the body of an adult animal is represented by: red bone marrow - a source of stem cells for immunocytes, central authorities lymphocytopoiesis (thymus), peripheral organs of lymphocytopoiesis (spleen, lymph nodes, accumulation of lymphoid tissue in organs), blood and lymph lymphocytes, as well as populations of lymphocytes and plasma cells penetrating all connective and epithelial tissues. All organs of the immune system function as a whole thanks to neurohumoral regulatory mechanisms, as well as the ongoing processes of migration and recirculation of cells through the circulatory and lymphatic systems. The main cells that exercise control and immunological protection in the body are lymphocytes, as well as plasma cells and macrophages.
3. There are two main types of lymphocytes: B-lymphocytes and T-lymphocytes. Stem cells and progenitor cells of B-lymphocytes are produced in the bone marrow. In mammals, differentiation of B-lymphocytes occurs here, characterized by the appearance of immunoglobulin receptors in cells. Further, such differentiated B-lymphocytes enter the peripheral lymphoid organs: the spleen, lymph nodes, lymph nodes of the digestive tract. In these organs, under the action of antigens, B-lymphocytes proliferate and further specialize with the formation of effector cells and memory B-cells.
T-lymphocytes also develop from stem cells of bone marrow origin. The latter are transferred with the blood flow to the thymus, turn into blasts, which divide and differentiate in two directions. Some blasts form a population of lymphocytes with special receptors that perceive foreign antigens. Differentiation of these cells occurs under the influence of a differentiation inductor produced and secreted by the epithelial elements of the thymus. The resulting T-lymphocytes (antigen-reactive lymphocytes) populate special T-zones (thymus-dependent) in the peripheral lymphoid organs. There, under the influence of antigens, they can undergo transformation into T-blasts, proliferate and differentiate into effector cells involved in transplantation (T-killers) and humoral immunity (T-helpers and T-suppressors), as well as into T-memory cells. Another part of T-blast descendants differentiate with the formation of cells carrying receptors for the antigens of their own organism. These cells are destroyed.
Thus, it is necessary to distinguish between antigen-independent and antigen-dependent proliferation, differentiation and specialization of B- and T-lymphocytes.
In the case of the formation of cellular immunity under the action of tissue antigens, the differentiation of T-lymphoblasts leads to the appearance of cytotoxic lymphocytes (T-killers) and memory T-cells. Cytotoxic lymphocytes are capable of destroying foreign cells (target cells) or through the secretion of special substances-mediators (lymphokines).
During the formation of humoral immunity, most soluble and other antigens also have a stimulating effect on T-lymphocytes; at the same time, T-helpers are formed that secrete mediators (lymphokines) that interact with B-lymphocytes and cause their transformation into B-blasts, which specialize in secreting plasma cell antibodies. The proliferation of antigen-stimulated T-lymphocytes also leads to an increase in the number of cells that turn into inactive small lymphocytes that retain information about this antigen for several years and are therefore called memory T-cells.
T-helper determines the specialization of B-lymphocytes in the direction of the formation of antibody-forming plasma cells, which provide “humoral immunity”, producing and releasing immunoglobulins into the blood. At the same time, the B-lymphocyte receives antigenic information from the macrophage, which captures the antigen, processes it and passes it on to the B-lymphocyte. On the surface of the B-lymphocyte there is a greater number of immunoglobulin receptors (50-150 thousand).
Thus, to ensure immunological reactions, the cooperation of the activities of the three main types of cells is necessary: B-lymphocytes, macrophages and T-lymphocytes (Fig. 13).
4. Macrophages play an important role in both natural and acquired immunity of the body. The participation of macrophages in natural immunity is manifested in their ability to phagocytosis. Their role in acquired immunity consists in the passive transfer of antigen to immunocompetent cells (T- and B-lymphocytes), in the induction of a specific response to antigens.
Most of the processed antigen material secreted by macrophages has a stimulating effect on the proliferation and differentiation of T- and B-lymphocyte clones.
In the B-zones of the lymph nodes and spleen, there are specialized macrophages (dendritic cells), on the surface of numerous processes of which many antigens are stored that enter the body and are transmitted to the corresponding clones of B-lymphocytes. In the T-zones of lymphatic follicles, interdigitating cells are located that affect the differentiation of T-lymphocyte clones.
Thus, macrophages are directly involved in the cooperative interaction of cells (T- and B-lymphocytes) in the body's immune responses.
There are two types of migration of cells of the immune system: slow and fast. The first is more typical for B-lymphocytes, the second - for T-lymphocytes. The processes of migration and recirculation of cells of the immune system ensure the maintenance of immune homeostasis.
See also the textbook "Methods for assessing the defense systems of the mammalian organism" (Katsy G.D., Koyuda L.I. - Lugansk. -2003. - p. 42-68).
Skeletal tissues: cartilage and bone
1. Development, structure and varieties of cartilage tissue.
2. Development, structure and types of bone tissue.
1. Cartilage tissue is a specialized type of connective tissue that performs a supporting function. In embryogenesis, it develops from the mesenchyme and forms the skeleton of the embryo, which is subsequently largely replaced by bone. Cartilage tissue, with the exception of the articular surfaces, is covered with dense connective tissue - the perichondrium, containing vessels that feed the cartilage and its cambial (chondrogenic) cells.
Cartilage consists of chondrocyte cells and intercellular substance. In accordance with the characteristics of the intercellular substance, there are three types of cartilage: hyaline, elastic and fibrous.
In the process of embryonic development of the embryo, the mesenchyme, intensively developing, forms islands of protochondral tissue cells tightly adjacent to each other. Its cells are characterized by high values of nuclear-cytoplasmic ratios, small dense mitochondria, an abundance of free ribosomes, poor development of granular EPS, etc. In the process of development, primary cartilaginous (prechondral) tissue is formed from these cells.
As the intercellular substance accumulates, the cells of the developing cartilage are isolated in separate cavities (lacunae) and differentiate into mature cartilage cells - chondrocytes.
Further growth of cartilage tissue is provided by the ongoing division of chondrocytes and the formation of an intercellular substance between daughter cells. The formation of the latter slows down over time. Daughter cells, remaining in one gap, form isogenic groups of cells (Isos - equal, genesis - origin).
As the cartilage tissue differentiates, the intensity of cell reproduction decreases, the nuclei become pictonized, and the nucleolar apparatus is reduced.
hyaline cartilage. In an adult organism, hyaline cartilage is part of the ribs, sternum, covers articular surfaces, etc. (Fig. 14).
Cartilage cells - chondrocytes - of its various zones have their own characteristics. So, immature cartilage cells - chondroblasts - are localized directly under the perichondrium. They are oval in shape, the cytoplasm is rich in RNA. In deeper areas of the cartilage, chondrocytes are rounded, forming characteristic “isogenic groups”.
The intercellular substance of hyaline cartilage contains up to 70% of the dry weight of the fibrillar collagen protein and up to 30% of the amorphous substance, which includes glycosaminoglycans, proteoglycans, lipids and non-collagen proteins.
The orientation of the fibers of the intercellular substance is determined by the laws of mechanical tension characteristic of each cartilage.
Collagen fibrils of cartilage, unlike collagen fibers of other types of connective tissue, are thin and do not exceed 10 nm in diameter.
Cartilage metabolism is ensured by the circulation of intercellular tissue fluid, which is up to 75% of the total tissue mass.
Elastic cartilage forms the skeleton of the outer ear, cartilage of the larynx. In addition to an amorphous substance and collagen fibrils, its composition includes a dense network of elastic fibers. Its cells are identical to those of hyaline cartilage. They also form groups and lie alone under the perichondrium (Fig. 15).
Fibrous cartilage is localized in the composition of the intervertebral discs, in the area of attachment of the tendon to the bones. The intercellular substance contains coarse bundles of collagen fibers. Cartilage cells form isogenic groups stretched into chains between bundles of collagen fibers (Fig. 16).
Cartilage regeneration is provided by the perichondrium, the cells of which retain cambiality - chondrogenic cells.
2. Bone tissue, like other types of connective tissue, develops from the mesenchyme and consists of cells and intercellular substance. It performs the function of support, protection and is actively involved in metabolism. In the spongy bone of the skeleton, the red bone marrow is localized, where the processes of hematopoiesis and differentiation of cells of the body's immune defense are carried out. The bone deposits salts of calcium, phosphorus, etc. Together minerals make up 65-70% of the dry weight of the fabric.
Bone tissue contains four different types of cells: osteogenic cells, osteoblasts, osteocytes, and osteoclasts.
Osteogenic cells are cells of an early stage of specific differentiation of the mesenchyme in the process of osteogenesis. They retain the potential for mitotic division. These cells are localized on the surface of the bone tissue: in the periosteum, endosteum, in Haversian canals and other areas of bone tissue formation. Reproducing, they replenish the supply of osteoblasts.
Osteoblasts are cells that produce organic elements of the intercellular substance of bone tissue: collagen, glycosaminoglycans, proteins, etc.
Osteocytes lie in special cavities of the intercellular substance - lacunae, interconnected by numerous bone tubules.
Osteoclasts are large, multinucleated cells. They are located on the surface of the bone tissue in the places of its resorption. Cells are polarized. The surface facing the resorbable tissue has a corrugated border due to thin branching processes.
The intercellular substance consists of collagen fibers and an amorphous substance: glycoproteins, glycosaminoglycans, proteins and inorganic compounds. 97% of all calcium in the body is concentrated in bone tissue.
In accordance with the structural organization of the intercellular substance, coarse-fibered bone and lamellar bone are distinguished (Fig. 17). Rough fibrous bone is characterized by a significant diameter of bundles of collagen fibrils and a variety of their orientation. It is typical for bones of an early stage of animal ontogeny. In lamellar bone, collagen fibrils do not form bundles. Being parallel, they form layers - bone plates with a thickness of 3-7 microns. In the plates there are cell cavities - lacunae and bone tubules connecting them, in which osteocytes and their processes lie. Tissue fluid circulates through the system of lacunae and tubules, which ensures the metabolism in the tissue.
Depending on the position of the bone plates, spongy and compact bone tissue is distinguished. In the spongy substance, in particular in the epiphyses of tubular bones, groups of bone plates are located at different angles to each other. Cancellous bone cells contain red bone marrow.
In a compact substance, groups of bone plates 4-15 microns thick are tightly adjacent to each other. Three layers are formed in the diaphysis: the outer common system of plates, the osteogenic layer, and the inner common system.
Perforating tubules pass through the external common system from the periosteum, carrying blood vessels and coarse bundles of collagen fibers into the bone.
In the osteogenic layer of the tubular bone, the osteon channels containing blood vessels and nerves are mainly oriented longitudinally. The system of tubular bone plates surrounding these channels - osteons contain from 4 to 20 plates. Osteons are delimited from each other by the cement line of the main substance; they are the structural unit of bone tissue (Fig. 18).
The internal common system of bone plates borders on the endosteum of the bone strip and is represented by plates oriented parallel to the canal surface.
There are two types of osteogenesis: directly from the mesenchyme ("direct") and by replacing embryonic cartilage with bone ("indirect") osteogenesis - fig. 19.20.
The first is characteristic for the development of coarse-fibered bones of the skull and lower jaw. The process begins with the intensive development of connective tissue and blood vessels. Mesenchymal cells, anastomosing with each other by processes, form a network. Cells pushed aside by the intercellular substance to the surface differentiate into osteoblasts, which are actively involved in osteogenesis. Subsequently, the primary coarse-fibered bone tissue is replaced by lamellar bone. The bones of the trunk, limbs, etc. are formed in place of cartilage tissue. In tubular bones, this process begins in the area of the diaphysis with the formation of a network of crossbars of coarse-fibered bone, the bone cuff, under the perichondrium. The process of replacing cartilage with bone tissue is called endochondral ossification.
Simultaneously with the development of the endochondral bone from the side of the periosteum, an active process of perichondral osteogenesis takes place, forming a dense layer of the periosteal bone, extending along its entire length to the epiphyseal growth plate. The periosteal bone is a compact bone substance of the skeleton.
Later, ossification centers appear in the epiphyses of the bone. Bone tissue here replaces cartilage. The latter is preserved only on the articular surface and in the epiphyseal growth plate, which delimits the epiphysis from the diaphysis during the entire period of growth of the organism until the puberty of the animal.
The periosteum (periosteum) consists of two layers: the inner one contains collagen and elastic fibers, osteoblasts, osteoclasts and blood vessels. External - formed by dense connective tissue. It is directly related to the tendons of the muscles.
Endooste - a layer of connective tissue lining the bone marrow canal. It contains osteoblasts and thin bundles of collagen fibers that pass into the tissue of the bone marrow.
Muscle tissues
1. Smooth.
2. Cardiac striated.
3. Skeletal striated.
4. Development, growth and regeneration of muscle fibers.
1. The leading function of muscle tissues is to ensure movement in space of the body as a whole and its parts. All muscle tissues make up a morphofunctional group, and depending on the structure of contraction organelles, it is divided into three groups: smooth, skeletal striated and cardiac striated muscle tissues. These tissues do not have a single source of embryonic development. They are mesenchyme, myotomes of segmented mesoderm, visceral leaf of splanchnotome, etc.
Smooth muscle tissue of mesenchymal origin. The tissue consists of myocytes and a connective tissue component. A smooth myocyte is a fusiform cell 20–500 µm long and 5–8 µm thick. The rod-shaped nucleus is located in its central part. There are many mitochondria in the cell.
Each myocyte is surrounded by a basement membrane. It has openings in the region of which slit-like junctions (nexuses) are formed between neighboring myocytes, providing functional interactions of myocytes in the tissue. Numerous reticular fibrils are woven into the basement membrane. Around muscle cells, reticular, elastic and thin collagen fibers form a three-dimensional network - endomysium, which unites neighboring myocytes.
Physiological regeneration of smooth muscle tissue usually manifests itself under conditions of increased functional loads, mainly in the form of compensatory hypertrophy. This is most clearly observed in the muscular membrane of the uterus during pregnancy.
Elements of muscle tissue of epidermal origin are myoepithelial cells that develop from the ectoderm. They are located in sweat, mammary, salivary and lacrimal glands, differentiating simultaneously with their secretory epithelial cells from common precursors. By contracting, the cells contribute to the excretion of the secretion of the gland.
Smooth muscles form muscle layers in all hollow and tubular organs.
2. The sources of development of cardiac striated muscle tissue are symmetrical sections of the visceral leaf of the splanchnotome. Most of its cells differentiate into cardiomyocytes (cardiac myocytes), the rest into epicardial mesothelial cells. Both have common progenitor cells. During histogenesis, several types of cardiomyocytes are differentiated: contractile, conductive, transitional and secretory.
The structure of contractile cardiomyocytes. Cells have an elongated shape (100-150 microns), close to cylindrical. Their ends are connected to each other by intercalary discs. The latter perform not only a mechanical function, but also conductive, provide an electrical connection between cells. The nucleus is oval in shape, located in the central part of the cell. It has a lot of mitochondria. They form chains around special organelles - myofibrils. The latter are built from permanently existing ordered filaments of actin and myosin - contractile proteins. To fix them, special structures are used - the telophragm and mesophragm, built from other proteins.
The section of the myofibril between the two Z-lines is called the sarcomere. A-bands - anisotropic, thick microfilaments, contain myosin: I-bands - isotropic, thin microfilaments, contain actin; The H-band is located in the middle of the A-band (Fig. 21).
There are several theories for the mechanism of myocyte contraction:
1) Under the influence of an action potential that propagates through the cytolemma, calcium ions are released, enter the myofibrils and initiate a contractile act, which is the result of the interaction of actin and myosin microfilaments; 2) The most common theory at present is the sliding thread model (G. Huxley, 1954). We are supporters of the latter.
Structural features of conducting cardiomyocytes. Cells are larger than working cardiomyocytes (length about 100 microns, and thickness about 50 microns). The cytoplasm contains all organelles of general importance. Myofibrils are few and lie along the periphery of the cell. These cardiomyocytes are connected into fibers with each other not only at the ends, but also at the side surfaces. The main function of conducting cardiomyocytes is that they perceive control signals from pacemaker elements and transmit information to contractile cardiomyocytes (Fig. 22).
In the definitive state, cardiac muscle tissue retains neither stem cells nor progenitor cells, so if cardiomyocytes die (heart attack), they do not regenerate.
3. The source of development of elements of skeletal striated muscle tissue are myocyte cells. Some of them differentiate in situ, while others migrate from the myotomes to the mesenchyme. The former are involved in the formation of the myosymplast, the latter differentiate into myosatellitocytes.
The main element of skeletal muscle tissue is a muscle fiber formed by myosymplast and myosatellitocytes. The fiber is surrounded by a sarcolemma. Since the symplast is not a cell, the term “cytoplasm” is not used, but they say “sarcoplasm” (Greek sarcos - meat). In the sarcoplasm, at the poles of the nuclei, organelles of general importance are located. Special organelles are represented by myofibrils.
The mechanism of fiber contraction is the same as in cardiomyocytes.
Inclusions, primarily myoglobin and glycogen, play an important role in the activity of muscle fibers. Glycogen serves as the main source of energy necessary both for performing muscle work and for maintaining the thermal balance of the whole organism.

Rice. 22. Ultramicroscopic structure of three types of cardiomyocytes: conducting (A), intermediate (B) and working (C) (scheme by G.S. Katinas)
1 - basement membrane; 2 - cell nuclei; 3 - myofibrils; 4 - plasmalemma; 5 - connection of working cardiomyocytes (insertion disk); connections of an intermediate cardiomyocyte with a working and conducting cardiomyocytes; 6 - connection of conducting cardiomyocytes; 7 - transverse tubule systems (general purpose organelles not shown).
Myosatellitocytes are adjacent to the surface of the symplast so that their plasma membranes are in contact. A significant number of satellite cells are associated with one symplast. Each myosatellitocyte is a mononuclear cell. The nucleus is smaller than the nucleus of the myosymplast and more rounded. Mitochondria and the endoplasmic reticulum are evenly distributed in the cytoplasm, the Golgi complex and the cell center are located next to the nucleus. Myosatellitocytes are the cambial elements of skeletal muscle tissue.
Muscle as an organ. Between the muscle fibers are thin layers of loose connective tissue - endomysium. Its reticular and collagen fibers intertwine with the fibers of the sarcolemma, which contributes to the unification of efforts during contraction. Muscle fibers are grouped into bundles, between which there are thicker layers of loose connective tissue - perimysium. It also contains elastic fibers. The connective tissue surrounding the muscle as a whole is called the epimysium.
Vascularization. The arteries entering the muscle branch in the perimysium. Next to them are many tissue basophils that regulate the permeability of the vascular wall. The capillaries are located in the endomysium. Venules and veins lie in the perimysium next to arterioles and arteries. This is where the lymphatic vessels pass.
Innervation. The nerves entering the muscle contain both efferent and afferent fibers. The process of a nerve cell, which brings an efferent nerve impulse, penetrates through the basement membrane and branches between it and the symplast plasmolemma, participating in the formation of a motor or motor plaque. The nerve impulse releases mediators here, which cause excitation that propagates along the symplast plasmalemma.
So, each muscle fiber is innervated independently and surrounded by a network of hemocapillaries. This complex forms the morphofunctional unit of the skeletal muscle - mion; sometimes the muscle fiber itself is called a myon, which does not correspond to the International Histological Nomenclature.
4. Cells from which striated muscle fibers are formed in embryogenesis are called myoblasts. After a series of divisions, these single-nuclear cells, which do not contain myofibrils, begin to merge with each other, forming elongated multinuclear cylindrical formations - microtubules, in which myofibrils and other organelles characteristic of striated muscle fibers appear in due time. In mammals, most of these fibers are formed before birth. During postnatal growth, muscles must become longer and thicker in order to maintain proportion to the growing skeleton. Their final value depends on the work that falls to their share. After the first year of life, further muscle growth is entirely due to the thickening of individual fibers, i.e., it represents hypertrophy (hyper - over, over and trophy - nutrition), and not an increase in their number, which would be called hyperplasia (from plasis - formation).
Thus, striated muscle fibers grow in thickness by increasing the number of myofibrils (and other organelles) they contain.
Muscle fibers lengthen as a result of fusion with satellite cells. In addition, in the postnatal period, elongation of myofibrils is possible by adding new sarcomeres to their ends.
Regeneration. Satellite cells not only provide one of the mechanisms for the growth of striated muscle fibers, but also remain a potential source of new myoblasts throughout life, the fusion of which can lead to the formation of completely new muscle fibers. Satellite cells are able to divide and give rise to myoblasts after muscle injury and in some dystrophic conditions, when there are attempts to regenerate new fibers. However, even minor defects in muscle tissue after severe injuries are filled with fibrous tissue formed by fibroblasts.
Growth and regeneration of smooth muscles. Like other muscle types, smooth muscles respond to increased functional demands with compensatory hypertrophy, but this is not the only possible response. For example, during pregnancy, not only the size of smooth muscle cells in the uterine wall (hypertrophy) increases, but also their number (hyperplasia).
In animals during pregnancy or after the administration of hormones, mitotic figures can often be seen in the muscle cells of the uterus; therefore, it is generally accepted that smooth muscle cells retain the ability to mitotic division.
nervous tissue
1. Tissue development.
2. Classification of nerve cells.
3. Neuroglia, its variety.
4. Synapses, fibers, nerve endings.
1. Nervous tissue - a specialized tissue that forms the main integrating system of the body - the nervous system. The main function is conductivity.
Nervous tissue consists of nerve cells - neurons that perform the function of nervous excitation and conduction of a nerve impulse, and neuroglia that provide support, trophic and protective functions.
Nervous tissue develops from the dorsal thickening of the ectoderm - the neural plate, which in the process of development differentiates into the neural tube, neural crests (rollers) and neural placodes.
In subsequent periods of embryogenesis, the brain and spinal cord form from the neural tube. The neural crest forms sensory ganglia, ganglia of the sympathetic nervous system, melanocytes of the skin, etc. The neural placodes are involved in the formation of the organs of smell, hearing, and sensory ganglia.
The neural tube consists of a single layer of prismatic cells. The latter, multiplying, form three layers: inner - ependymal, middle - mantle and outer - marginal veil.
Subsequently, the cells of the inner layer produce ependymal cells lining the central canal. spinal cord. The cells of the mantle layer differentiate into neuroblasts, which further turn into neurons and spongioblasts, giving rise to various types of neuroglia (astrocytes, oligodendrocytes).
2. Nerve cells (neurocytes, neurons) of various parts of the nervous system are characterized by a variety of shapes, sizes and functional significance. In accordance with the function, nerve cells are divided into receptor (afferent), associative and effector (efferent).
With a wide variety of forms of nerve cells, a common morphological feature is the presence of processes that ensure their connection as part of reflex arcs. The length of the processes is different and ranges from a few microns to 1-1.5 m.
The processes of nerve cells are divided into two types according to their functional significance. Some receive nervous excitation and conduct it to the perikaryon of the neuron. They are called dendrites. Another type of processes conducts an impulse from the cell body and transmits it to another neurocyte or to an axon (axos - axis), or neurite. All nerve cells have only one neurite.
According to the number of processes, nerve cells are divided into unipolar - with one process, bipolar and multipolar (Fig. 23).
The nuclei of nerve cells are large, rounded or slightly oval, located in the center of the perikaryon.
The cytoplasm of cells is characterized by an abundance of various organelles, neurofibrils, and chromatophilic substances. The surface of the cell is covered with a plasmalemma, which is characterized by excitability and the ability to conduct excitation.

Rice. 23. Types of nerve cells (scheme according to T.N. Radostina, L.S. Rumyantseva)
A - unipolar neuron; B - pseudounipolar neuron; B - bipolar neuron; D - multipolar neuron.
Neurofibrils are a collection of fibers, structures of the cytoplasm, forming a dense plexus in the perikaryon.
Chromatophilic (basophilic) substance is detected in the perikaryon of nephrocytes and in their dendrites, but is absent in axons.
Ependymocytes line the cavities of the central nervous system: the ventricles of the brain and the spinal canal. Cells facing the cavity of the neural tube contain cilia. Their opposite poles pass into long processes that support the backbone of the tissues of the neural tube. Ependymocytes are involved in the secretory function, releasing various active substances.
Astrocytes are either protoplasmic (short-beamed) or fibrous (long-beamed). The first are localized in the gray matter of the CNS (central nervous system). They are involved in the metabolism of the nervous tissue and perform a delimiting function.
Fibrous astrocytes are characteristic of the white matter of the CNS. They form the supporting apparatus of the CNS.
Oligodendrocytes are a large group of CNS and PNS (peripheral nervous system) cells. They surround the bodies of neurons, are part of the sheaths of nerve fibers and nerve endings, and participate in their metabolism.
Microglia (glial macrophages) is a specialized system of macrophages that performs a protective function. They develop from the mesenchyme, are capable of amoeboid movement. They are characteristic of the white and gray matter of the CNS.
4. The processes of nerve cells, together with the neuroglia that cover them, form nerve fibers. The processes of nerve cells located in them are called axial cylinders, and the oligodendroglia cells covering them are called neurolemmocytes (Schwann cells).
Distinguish between myelinated and non-myelinated nerve fibers.
Non-myelinated (non-myelinated) nerve fibers are characteristic of the autonomic nervous system. Lemmocytes fit tightly to each other, forming continuous strands. The fiber contains several axial cylinders, i.e., processes of various nerve cells. The plasmalemma forms deep folds that form a double membrane - the mesaxon, on which the axial cylinder is suspended. With light microscopy, these structures are not detected, which creates the impression of immersion of axial cylinders directly into the cytoplasm of glial cells.
Myelinated (pulp) nerve fibers. Their diameter ranges from 1 to 20 µm. They contain one axial cylinder - the dendrite or neurite of the nerve cell, covered with a sheath formed by lemmocytes. In the fiber sheath, two layers are distinguished: the inner one is myelin, thicker and the outer one is thin, containing the cytoplasm and nuclei of lemmocytes.
At the border of two lemmocytes, the myelin fiber sheath becomes thinner, a narrowing of the fiber is formed - a nodal interception (Ranvier intercept). The section of the nerve fiber between two intercepts is called the internodal segment. Its shell corresponds to one lemmocyte.
Nerve endings are different in their functional significance. There are three types of nerve endings: effector, receptor and end devices.
Effector nerve endings - these include motor nerve endings of striated and smooth muscles and secretory endings of glandular organs.
Motor nerve endings of striated skeletal muscles - motor plaques - a complex of interconnected structures of nervous and muscle tissues.
Sensory nerve endings (receptors) are specialized terminal formations of dendrites of sensitive neurons. There are two large groups of receptors: exteroreceptors and interoreceptors. Sensory endings are divided into mechanoreceptors, chemoreceptors, thermoreceptors, etc. They are divided into free and non-free nerve endings. The latter are covered with a connective tissue capsule and are called encapsulated. This group includes lamellar bodies (Fater-Pacini bodies), tactile bodies (Meissner bodies), etc.
Lamellar bodies are characteristic of the deep layers of the skin and internal organs. Tactile bodies are also formed by glial cells.
Synapses are a specialized contact of two neurons, providing one-way conduction of nervous excitation. Morphologically, in the synapse, the presynaptic and postsynaptic poles are distinguished, and there is a gap between them. There are synapses with chemical and electrical transmission.
According to the place of contact, synapses are distinguished: axosomatic, axodendrial and axoaxonal.
The presynaptic pole of the synapse is characterized by the presence of synaptic vesicles containing a mediator (acetylcholine or norepinephrine).
The nervous system is represented by sensory and motor cells, united by interneuronal synapses into functionally active formations - reflex arcs. A simple reflex arc consists of two neurons - sensory and motor.
The reflex arcs of higher vertebrates still contain a significant number of associative neurons located between sensory and motor neurons.
A nerve is a bundle of fibers surrounded by a dense sheath of the perineurium. Small nerves consist of only one bundle surrounded by endoneurium. The number and diameter of nerve fibers in the bundle are very variable. There are more fibers in the distal portions of some nerves than in the more proximal portions. This is due to the branching of the fibers.
Blood supply to the nerves. The nerves are abundantly supplied with vessels that form many anastomoses. There are epineural, interfascicular, perineural and intrafascicular arteries and arterioles. The endoneurium contains a network of capillaries.
Literature
1. Alexandrovskaya O.V., Radostina T.N., Kozlov N.A. Cytology, histology and embryology.-M: Agropromizdat, 1987.- 448 p.
2. Afanasiev Yu.I., Yurina N.A. Histology.- M: Medicine, 1991.- 744 p.
3. Vrakin V.F., Sidorova M.V. Morphology of farm animals. - M: Agropromizdat, 1991.- 528 p.
4. Glagolev P.A., Ippolitova V.I. Anatomy of farm animals with the basics of histology and embryology.- M: Kolos, 1977.- 480 p.
5. Ham A., Cormac D. Histology. -M: Mir, 1982.-T 1-5.
6. Seravin L.N. The origin of the eukaryotic cell //Citology.-1986/-T. 28.-No. 6-8.
7. Seravin L.N. The main stages in the development of cell theory and the place of the cell among living systems //Citology.-1991.-V.33.-№ 12/-C. 3-27.
HISTOLOGY
the science that studies animal tissues. A tissue is a group of cells that are similar in shape, size and function and in their metabolic products. In all plants and animals, with the exception of the most primitive, the body consists of tissues, and in higher plants and in highly organized animals, tissues are distinguished by a great variety of structure and the complexity of their products; combining with each other, different tissues form separate organs of the body. Histology is the study of animal tissues; the study of plant tissues is usually referred to as plant anatomy. Histology is sometimes called microscopic anatomy, because it studies the structure (morphology) of an organism at the microscopic level (very thin tissue sections and individual cells serve as the object of histological examination). Although this science is primarily descriptive, its task also includes the interpretation of those changes that occur in tissues in normal and pathological conditions. Therefore, the histologist needs to be well versed in how tissues are formed in the process of embryonic development, what is their ability to grow in the postembryonic period, and how they undergo changes in various natural and experimental conditions, including during their aging and the death of their constituent cells. The history of histology as a separate branch of biology is closely connected with the creation of the microscope and its improvement. M. Malpighi (1628-1694) is called the "father of microscopic anatomy", and hence histology. Histology was enriched by the observations and methods of research carried out or created by many scientists whose main interests lay in the field of zoology or medicine. This is evidenced by the histological terminology that immortalized their names in the names of the structures they first described or the methods they created: islets of Langerhans, Lieberkühn glands, Kupffer cells, Malpighian layer, Maximov stain, Giemsa stain, etc. At present, methods for preparing preparations and their microscopic examination have become widespread, making it possible to study individual cells. These methods include frozen section technique, phase contrast microscopy, histochemical analysis, tissue culture, electron microscopy; the latter allows a detailed study of cellular structures (cell membranes, mitochondria, etc.). Using a scanning electron microscope, it was possible to reveal an interesting three-dimensional configuration of free surfaces of cells and tissues, which cannot be seen under a conventional microscope.
Origin of tissues. The development of an embryo from a fertilized egg occurs in higher animals as a result of multiple cell divisions (crushing); the cells formed in this case are gradually distributed in their places in different parts of the future embryo. Initially, embryonic cells are similar to each other, but as their number increases, they begin to change, acquiring characteristic features and the ability to perform certain tasks. specific functions. This process, called differentiation, eventually leads to the formation of different tissues. All tissues of any animal come from three initial germ layers: 1) the outer layer, or ectoderm; 2) the innermost layer, or endoderm; and 3) the middle layer, or mesoderm. So, for example, muscles and blood are derivatives of the mesoderm, the lining of the intestinal tract develops from the endoderm, and the ectoderm forms integumentary tissues and the nervous system.
See also EMBRYOLOGY.
main types of fabrics. Histologists usually distinguish four main tissues in humans and higher animals: epithelial, muscular, connective (including blood), and nervous. In some tissues, cells have approximately the same shape and size and are so tightly adjacent to one another that there is no or almost no intercellular space between them; such tissues cover the outer surface of the body and line its internal cavities. In other tissues (bone, cartilage), the cells are not so densely packed and are surrounded by the intercellular substance (matrix) that they produce. From the cells of the nervous tissue (neurons) that form the brain and spinal cord, long processes depart, ending very far from the cell body, for example, at the points of contact with muscle cells. Thus, each tissue can be distinguished from others by the nature of the location of the cells. Some tissues have a syncytial structure, in which the cytoplasmic processes of one cell pass into similar processes of neighboring cells; such a structure is observed in the germinal mesenchyme, loose connective tissue, reticular tissue, and can also occur in some diseases. Many organs are composed of several types of tissues, which can be recognized by their characteristic microscopic structure. Below is a description of the main types of tissues found in all vertebrates. Invertebrates, with the exception of sponges and coelenterates, also have specialized tissues similar to the epithelial, muscular, connective, and nervous tissues of vertebrates.
epithelial tissue. The epithelium may consist of very flat (scaly), cuboidal, or cylindrical cells. Sometimes it is multi-layered, i.e. consisting of several layers of cells; such an epithelium forms, for example, the outer layer of the human skin. In other parts of the body, for example in the gastrointestinal tract, the epithelium is single-layered, i.e. all of its cells are connected to the underlying basement membrane. In some cases, a single-layer epithelium may appear to be multi-layered: if the long axes of its cells are not parallel to each other, then it seems that the cells are at different levels, although in fact they lie on the same basement membrane. Such an epithelium is called multilayered. The free edge of epithelial cells is covered with cilia, i.e. thin hair-like outgrowths of protoplasm (such a ciliary epithelium lines, for example, the trachea), or ends with a "brush border" (the epithelium lining the small intestine); this border consists of ultramicroscopic finger-like outgrowths (so-called microvilli) on the cell surface. In addition to protective functions, the epithelium serves as a living membrane through which gases and solutes are absorbed by cells and released to the outside. In addition, the epithelium forms specialized structures, such as glands that produce substances necessary for the body. Sometimes secretory cells are scattered among other epithelial cells; an example is the mucus-producing goblet cells in the surface layer of the skin in fish or in the intestinal lining in mammals.

Muscle. Muscle tissue differs from the rest in its ability to contract. This property is due to the internal organization of muscle cells containing a large number of submicroscopic contractile structures. There are three types of muscles: skeletal, also called striated or voluntary; smooth, or involuntary; cardiac muscle, which is striated but involuntary. Smooth muscle tissue consists of spindle-shaped mononuclear cells. The striated muscles are formed from multinuclear elongated contractile units with a characteristic transverse striation, i.e. alternating light and dark stripes perpendicular to the long axis. The cardiac muscle consists of mononuclear cells, connected end to end, and has a transverse striation; while the contractile structures of neighboring cells are connected by numerous anastomoses, forming a continuous network.

Connective tissue. There are different types of connective tissue. The most important supporting structures of vertebrates consist of two types of connective tissue - bone and cartilage. Cartilage cells (chondrocytes) secrete around themselves a dense elastic ground substance (matrix). Bone cells (osteoclasts) are surrounded by a ground substance containing salt deposits, mainly calcium phosphate. The consistency of each of these tissues is usually determined by the nature of the basic substance. As the body ages, the content of mineral deposits in the ground substance of the bone increases, and it becomes more brittle. In young children, the basic substance of the bone, as well as cartilage, is rich organic matter; due to this, they usually have not real bone fractures, but the so-called. fractures (fractures of the "green branch" type). Tendons are made up of fibrous connective tissue; its fibers are formed from collagen, a protein secreted by fibrocytes (tendon cells). Adipose tissue is located in different parts of the body; This is a peculiar type of connective tissue, consisting of cells, in the center of which there is a large globule of fat.

Blood. Blood is a very special type of connective tissue; some histologists even distinguish it as an independent type. The blood of vertebrates consists of liquid plasma and formed elements: red blood cells, or erythrocytes containing hemoglobin; a variety of white cells, or leukocytes (neutrophils, eosinophils, basophils, lymphocytes, and monocytes), and platelets, or platelets. In mammals, mature erythrocytes entering the bloodstream do not contain nuclei; in all other vertebrates (fish, amphibians, reptiles, and birds), mature, functioning erythrocytes contain a nucleus. Leukocytes are divided into two groups - granular (granulocytes) and non-granular (agranulocytes) - depending on the presence or absence of granules in their cytoplasm; in addition, they are easy to differentiate using staining with a special mixture of dyes: eosinophil granules acquire a bright pink color with this staining, the cytoplasm of monocytes and lymphocytes - a bluish tint, basophil granules - a purple tint, neutrophil granules - a faint purple tint. In the bloodstream, the cells are surrounded by a transparent liquid (plasma) in which various substances are dissolved. Blood delivers oxygen to tissues, removes carbon dioxide and metabolic products from them, and carries nutrients and secretion products, such as hormones, from one part of the body to another. See also BLOOD.

nervous tissue. Nervous tissue consists of highly specialized cells - neurons, concentrated mainly in the gray matter of the brain and spinal cord. A long process of a neuron (axon) stretches for long distances from the place where the body of the nerve cell containing the nucleus is located. The axons of many neurons form bundles, which we call nerves. Dendrites also depart from neurons - shorter processes, usually numerous and branched. Many axons are covered by a special myelin sheath, which is made up of Schwann cells containing a fat-like material. Neighboring Schwann cells are separated by small gaps called nodes of Ranvier; they form characteristic depressions on the axon. Nervous tissue is surrounded by a special type of supporting tissue known as neuroglia.


 A tissue is a system of cells and their derivatives (fibers, amorphous substance, syncytia, symplasts) that has arisen in the process of development and is characterized by common morphophysiological properties. Syncytium is called a mesh structure consisting of cells, the processes of which are closely interconnected. A symplast is a structure consisting of many cells that have merged with each other (this is how striated muscle tissue is built).
A tissue is a system of cells and their derivatives (fibers, amorphous substance, syncytia, symplasts) that has arisen in the process of development and is characterized by common morphophysiological properties. Syncytium is called a mesh structure consisting of cells, the processes of which are closely interconnected. A symplast is a structure consisting of many cells that have merged with each other (this is how striated muscle tissue is built).
 All types of tissues are combined into four main groups: 1) epithelial, 2) support-trophic, 3) muscle, 4) nervous tissue.
All types of tissues are combined into four main groups: 1) epithelial, 2) support-trophic, 3) muscle, 4) nervous tissue.
 Epithelial tissues Everywhere on the border between the organism and the environment, separating it from the environment - it covers the body from the surface in a continuous layer and lines the internal organs - there is epithelial tissue.
Epithelial tissues Everywhere on the border between the organism and the environment, separating it from the environment - it covers the body from the surface in a continuous layer and lines the internal organs - there is epithelial tissue.
 All epithelia are built from epithelial cells - epitheliocytes. Epitheliocytes are connected to each other with the help of desmosomes, closure bands, gluing bands, forming a cell layer. Epithelial layers are attached to the basement membrane, and through it to the connective tissue that feeds the epithelium.
All epithelia are built from epithelial cells - epitheliocytes. Epitheliocytes are connected to each other with the help of desmosomes, closure bands, gluing bands, forming a cell layer. Epithelial layers are attached to the basement membrane, and through it to the connective tissue that feeds the epithelium.
 The basement membrane consists of an amorphous substance and fibrillar structures. The functions of the basement membrane are the transport of macromolecular compounds and the creation of an elastic basis for epithelial cells. The tissue does not have blood vessels, there are no non-cellular forms of living matter. Epithelial cells are fed by tissue fluid coming from the connective tissue.
The basement membrane consists of an amorphous substance and fibrillar structures. The functions of the basement membrane are the transport of macromolecular compounds and the creation of an elastic basis for epithelial cells. The tissue does not have blood vessels, there are no non-cellular forms of living matter. Epithelial cells are fed by tissue fluid coming from the connective tissue.
 Depending on the location and function performed, two types of epithelium are distinguished: integumentary and glandular.
Depending on the location and function performed, two types of epithelium are distinguished: integumentary and glandular.
 By the nature of the location of the cells, the integumentary epithelium is divided into: single-layer (consists of a single layer of cells attached to the basement membrane by the lower poles) multilayer (only the lower cells lie on the basement membrane, and all the rest are located on the underlying epithelial cells).
By the nature of the location of the cells, the integumentary epithelium is divided into: single-layer (consists of a single layer of cells attached to the basement membrane by the lower poles) multilayer (only the lower cells lie on the basement membrane, and all the rest are located on the underlying epithelial cells).
 Single-layer epithelium single-row (free ends of cells and nuclei are located at the same level) multi-row (all cells lie on the basement membrane, but the nuclei are at different heights from it, resulting in a multi-row effect)
Single-layer epithelium single-row (free ends of cells and nuclei are located at the same level) multi-row (all cells lie on the basement membrane, but the nuclei are at different heights from it, resulting in a multi-row effect)

 Integumentary epithelium (scheme according to Aleksandrovskaya): single-layer (simple): A - flat (squamous); B - cubic; B - cylindrical (columnar); G - multi-row cylindrical ciliated (pseudo-multilayer): 1 - ciliated cell; 2 - shimmering cilia; 3 - insert (replacement) cell;
Integumentary epithelium (scheme according to Aleksandrovskaya): single-layer (simple): A - flat (squamous); B - cubic; B - cylindrical (columnar); G - multi-row cylindrical ciliated (pseudo-multilayer): 1 - ciliated cell; 2 - shimmering cilia; 3 - insert (replacement) cell;
 The single-layer squamous epithelium of the serous membranes (pleura and peritoneum) is called the mesothelium, the inner walls of the blood vessels, the alveoli of the lungs and the retina of the eyes are called the endothelium.
The single-layer squamous epithelium of the serous membranes (pleura and peritoneum) is called the mesothelium, the inner walls of the blood vessels, the alveoli of the lungs and the retina of the eyes are called the endothelium.
 Single-layer squamous epithelium (mesothelium) from the serous membrane of the omentum Designations: 1 - cell borders; 2 - nuclei of mesotheliocytes; 3 - binuclear cells; 4 - "hatches" The drug is a thin film, the basis of which is loose connective tissue, covered on both sides with a single-layer squamous epithelium - mesothelium. Mesothelial cells are flat, large, with light cytoplasm and rounded nuclei. Cell borders have a jagged appearance and are clearly contrasted by the black silver deposit. In some places between the cells there are small holes - HATCHES.
Single-layer squamous epithelium (mesothelium) from the serous membrane of the omentum Designations: 1 - cell borders; 2 - nuclei of mesotheliocytes; 3 - binuclear cells; 4 - "hatches" The drug is a thin film, the basis of which is loose connective tissue, covered on both sides with a single-layer squamous epithelium - mesothelium. Mesothelial cells are flat, large, with light cytoplasm and rounded nuclei. Cell borders have a jagged appearance and are clearly contrasted by the black silver deposit. In some places between the cells there are small holes - HATCHES.
 A single-layer cubic epithelium is found in the ducts of the glands, in the tubules of the kidneys, follicles of the thyroid gland. A single-layer prismatic epithelium is found in the mucous membrane of the intestines, stomach, uterus, oviducts, as well as in the excretory ducts of the liver, pancreas. Varieties of prismatic epithelium include limbic (intestinal epithelium) and glandular (stomach epithelium).
A single-layer cubic epithelium is found in the ducts of the glands, in the tubules of the kidneys, follicles of the thyroid gland. A single-layer prismatic epithelium is found in the mucous membrane of the intestines, stomach, uterus, oviducts, as well as in the excretory ducts of the liver, pancreas. Varieties of prismatic epithelium include limbic (intestinal epithelium) and glandular (stomach epithelium).
 The multi-row ciliated epithelium bears 20,270 oscillating cilia at the free ends of the cells. With the help of their movements, solid or liquid foreign particles are removed from the respiratory tract and female genital organs.
The multi-row ciliated epithelium bears 20,270 oscillating cilia at the free ends of the cells. With the help of their movements, solid or liquid foreign particles are removed from the respiratory tract and female genital organs.
 Simple epithelium A - Squamous B - Single-layered cubic C - Cylindrical D - Cylindrical ciliated D - Sensory with special sensory outgrowths E - Glandular epithelium containing goblet cells that secrete mucus
Simple epithelium A - Squamous B - Single-layered cubic C - Cylindrical D - Cylindrical ciliated D - Sensory with special sensory outgrowths E - Glandular epithelium containing goblet cells that secrete mucus
 Stratified epithelium consists of several layers of cells Stratified, depending on the shape of the cells, stratified squamous keratinized stratified transitional non-keratinized
Stratified epithelium consists of several layers of cells Stratified, depending on the shape of the cells, stratified squamous keratinized stratified transitional non-keratinized
 Integumentary epithelium (scheme according to Aleksandrovskaya): multilayered: D - flat (squamous) non-keratinizing: 1 cells of the basal layer; 2 cells of spiny layer; 3 - cell of the surface layer; E - flat (squamous) keratinizing: 1 - basal layer; 2 - prickly; 3 - granular; 4 shiny; 5 horny; G - transitional: 1 cells of the basal layer; 2 - cells of the intermediate layer; 3 - cells of the integumentary layer. Solid arrow shows loose connective tissue, dashed arrow shows goblet cell
Integumentary epithelium (scheme according to Aleksandrovskaya): multilayered: D - flat (squamous) non-keratinizing: 1 cells of the basal layer; 2 cells of spiny layer; 3 - cell of the surface layer; E - flat (squamous) keratinizing: 1 - basal layer; 2 - prickly; 3 - granular; 4 shiny; 5 horny; G - transitional: 1 cells of the basal layer; 2 - cells of the intermediate layer; 3 - cells of the integumentary layer. Solid arrow shows loose connective tissue, dashed arrow shows goblet cell
 Non-keratinized epithelium is found in the cornea of the eyes, esophagus, and vagina. The keratinizing epithelium forms the surface layer of the skin - the epidermis, it also lines the mucous membrane of the oral cavity, pharynx, esophagus. The epithelium of this species consists of four layers of gradually keratinizing cells: the deepest layer is the growth layer, it consists of living cells that have not lost the ability to mitosis. granular layer stratum corneum stratum corneum consisting of horny scales
Non-keratinized epithelium is found in the cornea of the eyes, esophagus, and vagina. The keratinizing epithelium forms the surface layer of the skin - the epidermis, it also lines the mucous membrane of the oral cavity, pharynx, esophagus. The epithelium of this species consists of four layers of gradually keratinizing cells: the deepest layer is the growth layer, it consists of living cells that have not lost the ability to mitosis. granular layer stratum corneum stratum corneum consisting of horny scales


 Stratified squamous non-keratinized epithelium and glandular epithelium from a section of the esophagus of a dog Mucosa is lined with stratified squamous non-keratinized epithelium located on a wavy basement membrane. Designations: 1 - basement membrane; 2 - basal layer; 3 - prickly layer; 4 - surface layer; 5 - loose connective tissue; 6 - secretory sections of the mucous glands; 7 - excretory ducts of glands In the loose connective tissue of the mucous membrane there are complex branched tubular alveolar mucous glands. The excretory ducts look like tubes cut in different planes.
Stratified squamous non-keratinized epithelium and glandular epithelium from a section of the esophagus of a dog Mucosa is lined with stratified squamous non-keratinized epithelium located on a wavy basement membrane. Designations: 1 - basement membrane; 2 - basal layer; 3 - prickly layer; 4 - surface layer; 5 - loose connective tissue; 6 - secretory sections of the mucous glands; 7 - excretory ducts of glands In the loose connective tissue of the mucous membrane there are complex branched tubular alveolar mucous glands. The excretory ducts look like tubes cut in different planes.
 Stratified transitional epithelium lines the mucous membranes of the urinary tract. Since the volume of their cavities changes during the functioning of these organs, the thickness of the epithelial layer undergoes stretching and compression.
Stratified transitional epithelium lines the mucous membranes of the urinary tract. Since the volume of their cavities changes during the functioning of these organs, the thickness of the epithelial layer undergoes stretching and compression.
 Dog bladder. Transitional epithelium Designations: I - mucous membrane: 1 - transitional epithelium; 2 - own record; 3 - submucosal base; II - muscular membrane: 4 - inner longitudinal layer; 5 - middle circular layer; 6 - outer longitudinal layer; 7 - layers of loose connective tissue; 8 - vessels; III - outer shell
Dog bladder. Transitional epithelium Designations: I - mucous membrane: 1 - transitional epithelium; 2 - own record; 3 - submucosal base; II - muscular membrane: 4 - inner longitudinal layer; 5 - middle circular layer; 6 - outer longitudinal layer; 7 - layers of loose connective tissue; 8 - vessels; III - outer shell
 Glandular epithelium Cells of epithelial tissue are capable of synthesizing active substances (secretion, hormone) necessary for the implementation of the functions of other organs. The epithelium that produces secrets is called glandular, and its cells are called secretory cells (granulocytes).
Glandular epithelium Cells of epithelial tissue are capable of synthesizing active substances (secretion, hormone) necessary for the implementation of the functions of other organs. The epithelium that produces secrets is called glandular, and its cells are called secretory cells (granulocytes).
 Glands Endocrine endo - inside, krio - separate They are deprived of excretory ducts, their active substances (hormones) enter the blood through capillaries (thyroid gland, pituitary gland, adrenal glands). Exocrine exo from the outside Secrets are secreted by glands that have ducts (mammary, sweat, salivary glands).
Glands Endocrine endo - inside, krio - separate They are deprived of excretory ducts, their active substances (hormones) enter the blood through capillaries (thyroid gland, pituitary gland, adrenal glands). Exocrine exo from the outside Secrets are secreted by glands that have ducts (mammary, sweat, salivary glands).

 Types of glands (according to the method of secretion excretion) holocrine glands (in which complete destruction of cells and secretion is constantly taking place). For example, the sebaceous gland of the skin; apocrine glands (part of the cell is destroyed): macroapocrine (the apex of the glandulocyte is destroyed) microapocrine (the apical parts of the microvilli are separated). The apocrine glands are the mammary and sweat glands. merocrine (in which glandulocytes are not destroyed). This type of glands includes: salivary glands, pancreas, stomach glands, endocrine glands.
Types of glands (according to the method of secretion excretion) holocrine glands (in which complete destruction of cells and secretion is constantly taking place). For example, the sebaceous gland of the skin; apocrine glands (part of the cell is destroyed): macroapocrine (the apex of the glandulocyte is destroyed) microapocrine (the apical parts of the microvilli are separated). The apocrine glands are the mammary and sweat glands. merocrine (in which glandulocytes are not destroyed). This type of glands includes: salivary glands, pancreas, stomach glands, endocrine glands.
 Support-trophic (connective tissues) Ø blood Ø lymph Ø cartilage tissue Ø bone tissue This type includes tissues that form the skeleton of organs and the whole body of the animal, they constitute the internal environment of the body.
Support-trophic (connective tissues) Ø blood Ø lymph Ø cartilage tissue Ø bone tissue This type includes tissues that form the skeleton of organs and the whole body of the animal, they constitute the internal environment of the body.
 A common morphological feature of tissues is the presence in the composition of not only cells, but also intercellular substance. The main functions are supporting, trophic, biological protection of the body.
A common morphological feature of tissues is the presence in the composition of not only cells, but also intercellular substance. The main functions are supporting, trophic, biological protection of the body.

 Mesenchyme is the most primitive tissue, found only in embryos. It is built on the principle of syncytium (a set of embryonic reticularly connected process cells), in the intervals of which there is a gelatinous intercellular substance.
Mesenchyme is the most primitive tissue, found only in embryos. It is built on the principle of syncytium (a set of embryonic reticularly connected process cells), in the intervals of which there is a gelatinous intercellular substance.


 Lymph consists of a liquid part - lymphoplasm and formed elements of lymphocytes - Peripheral lymph (lymph capillaries and vessels to the lymph nodes) - Intermediate lymph (vascular lymph after passing through the lymph nodes) - Central lymph (lymph of the thoracic and right lymphatic ducts)
Lymph consists of a liquid part - lymphoplasm and formed elements of lymphocytes - Peripheral lymph (lymph capillaries and vessels to the lymph nodes) - Intermediate lymph (vascular lymph after passing through the lymph nodes) - Central lymph (lymph of the thoracic and right lymphatic ducts)
 Cartilage tissue Hyaline, or vitreous, cartilage (on the articular surfaces, tips of the ribs, in the nasal septum, trachea and bronchi) Elastic cartilage (in the auricle, in the epiglottis, external auditory canal) Fibrous cartilage (intervertebral discs, junctions from tendons to bones )
Cartilage tissue Hyaline, or vitreous, cartilage (on the articular surfaces, tips of the ribs, in the nasal septum, trachea and bronchi) Elastic cartilage (in the auricle, in the epiglottis, external auditory canal) Fibrous cartilage (intervertebral discs, junctions from tendons to bones )
 Hyaline cartilage 1 - perichondrium; 2 cartilage zone with young cartilage cells; 3 - basic substance; 4 - highly differentiated cartilage cells; 5 - isogenic groups of cartilage cells; 6 capsule cartilage cells; 7 Basophilic ground substance around cartilage cells
Hyaline cartilage 1 - perichondrium; 2 cartilage zone with young cartilage cells; 3 - basic substance; 4 - highly differentiated cartilage cells; 5 - isogenic groups of cartilage cells; 6 capsule cartilage cells; 7 Basophilic ground substance around cartilage cells
 Elastic cartilage of the auricle: 1 perichondrium; 2 - young cartilage cells; 3 - isogenic groups of cartilage cells; 4 - elastic fibers
Elastic cartilage of the auricle: 1 perichondrium; 2 - young cartilage cells; 3 - isogenic groups of cartilage cells; 4 - elastic fibers
 Fibrous cartilage at the site of attachment of the tendon to the tibia: 1 - tendon cells; 2 - cartilage cells
Fibrous cartilage at the site of attachment of the tendon to the tibia: 1 - tendon cells; 2 - cartilage cells
 Bone tissue (textus osseus) is a mineralized type of connective tissue containing in the dry mass almost 70% of inorganic compounds, mainly calcium phosphate. Performs supporting, mechanical, depot for calcium salts and protective for internal organs, functions.
Bone tissue (textus osseus) is a mineralized type of connective tissue containing in the dry mass almost 70% of inorganic compounds, mainly calcium phosphate. Performs supporting, mechanical, depot for calcium salts and protective for internal organs, functions.
 Depending on the structural features, two types of bone tissue are distinguished: coarse fibrous lamellar Coarse fibrous is an embryonic bone tissue with a large number of cellular elements and a disorderly arrangement of collagen fibers collected in bundles. Subsequently, the coarse fibrous tissue is replaced by lamellar bone tissue, consisting of cells and bone plates that have a certain spatial orientation, and the cells and collagen fibers in them are enclosed in a mineralized amorphous substance. A compact and spongy substance of flat and tubular bones of the skeleton is formed from lamellar bone tissue.
Depending on the structural features, two types of bone tissue are distinguished: coarse fibrous lamellar Coarse fibrous is an embryonic bone tissue with a large number of cellular elements and a disorderly arrangement of collagen fibers collected in bundles. Subsequently, the coarse fibrous tissue is replaced by lamellar bone tissue, consisting of cells and bone plates that have a certain spatial orientation, and the cells and collagen fibers in them are enclosed in a mineralized amorphous substance. A compact and spongy substance of flat and tubular bones of the skeleton is formed from lamellar bone tissue.
 Scheme of the structure of the tubular bone: 1 - periosteum; 2 - haversian channel; 3 - insert system; 4 - haversian system; 5 - external common system of bone plates; 6 - blood vessels; 7 Volkman channel; 8 - compact bone; 9 - spongy bone; 10 - internal common system of bone plates
Scheme of the structure of the tubular bone: 1 - periosteum; 2 - haversian channel; 3 - insert system; 4 - haversian system; 5 - external common system of bone plates; 6 - blood vessels; 7 Volkman channel; 8 - compact bone; 9 - spongy bone; 10 - internal common system of bone plates
 Connective tissue with special properties: reticular adipose pigmented mucosa It is characterized by the predominance of a certain type of cells
Connective tissue with special properties: reticular adipose pigmented mucosa It is characterized by the predominance of a certain type of cells
 Reticular tissue is formed by reticular cells and their derivatives - reticular fibers. Reticular tissue forms the stroma of hematopoietic organs and creates a microenvironment for blood cells and macrophages. Adipose tissue is a collection of fat cells that provide the synthesis and accumulation of lipids in the body. Distinguish between white and brown adipose tissue. Pigmented connective tissue is a loose fibrous connective tissue with a significant predominance of pigment cells. An example of pigment tissue is the tissue of the iris and choroid of the eye. Mucous connective tissue is present only in the embryonic period, it is found in many organs, especially under the skin. An example of mucosal tissue is the tissue of the umbilical cord in the fetus.
Reticular tissue is formed by reticular cells and their derivatives - reticular fibers. Reticular tissue forms the stroma of hematopoietic organs and creates a microenvironment for blood cells and macrophages. Adipose tissue is a collection of fat cells that provide the synthesis and accumulation of lipids in the body. Distinguish between white and brown adipose tissue. Pigmented connective tissue is a loose fibrous connective tissue with a significant predominance of pigment cells. An example of pigment tissue is the tissue of the iris and choroid of the eye. Mucous connective tissue is present only in the embryonic period, it is found in many organs, especially under the skin. An example of mucosal tissue is the tissue of the umbilical cord in the fetus.
 Muscle tissue Muscle tissue is a group of tissues heterogeneous in origin and structure, united by a single and for it the main functional feature - the ability to contract, which is accompanied by a change in membrane potential. Depending on the morphofunctional features of contraction organelles - myofibrils, muscle tissues are divided into: - non-striated (smooth) muscle tissues - striated (transverse cavity) muscle tissues - specialized contractile tissues of epidermal and neural origin
Muscle tissue Muscle tissue is a group of tissues heterogeneous in origin and structure, united by a single and for it the main functional feature - the ability to contract, which is accompanied by a change in membrane potential. Depending on the morphofunctional features of contraction organelles - myofibrils, muscle tissues are divided into: - non-striated (smooth) muscle tissues - striated (transverse cavity) muscle tissues - specialized contractile tissues of epidermal and neural origin

 Nervous tissue provides in the body the regulation of the interaction of various tissues and organs and communication with the environment based on excitation and impulse conduction through specialized structures. Nervous tissue is built from nerve cells (neurocytes, neurons) and neuroglia. The neuron is the main structural component of specialized tissue. Performs the function of conducting an impulse. Neuroglia performs trophic, delimiting, supporting, secretory and protective functions.
Nervous tissue provides in the body the regulation of the interaction of various tissues and organs and communication with the environment based on excitation and impulse conduction through specialized structures. Nervous tissue is built from nerve cells (neurocytes, neurons) and neuroglia. The neuron is the main structural component of specialized tissue. Performs the function of conducting an impulse. Neuroglia performs trophic, delimiting, supporting, secretory and protective functions.
 In neurons, a body or perikaryon, processes that form nerve fibers, and nerve endings are isolated. Neurons have a specialized plasmalemma capable of conducting excitation from processes to the body and from it to the process due to depolarization. Nerve processes are functionally divided into: axon, or neurite propagates an impulse from the body of a neuron to another neuron or to the tissues of the working organ to muscles, glands dendrite perceive irritation, form an impulse and conduct it to the body of a neuron
In neurons, a body or perikaryon, processes that form nerve fibers, and nerve endings are isolated. Neurons have a specialized plasmalemma capable of conducting excitation from processes to the body and from it to the process due to depolarization. Nerve processes are functionally divided into: axon, or neurite propagates an impulse from the body of a neuron to another neuron or to the tissues of the working organ to muscles, glands dendrite perceive irritation, form an impulse and conduct it to the body of a neuron
 The structure of the nerve cell: 1 - body (pericarion); 2 core; 3 - dendrites; 4 - neurites; 5, 8 - myelin sheath; 7 collateral; 9 node interception; 10 - lemmocyte; 11 - nerve endings
The structure of the nerve cell: 1 - body (pericarion); 2 core; 3 - dendrites; 4 - neurites; 5, 8 - myelin sheath; 7 collateral; 9 node interception; 10 - lemmocyte; 11 - nerve endings