The vestibular nerve (n. vestibularis) is part of a complex system that provides the function of regulating balance, statics and dynamics of the body in space (Fig. 11). The first neurons of the vestibular pathway lie in the vestibular ganglion ( ganglion vestibularis scarpe), located deep in the ear canal. The dendrites of the node cells end in receptors in the labyrinth: in the ampoules of the three semicircular canals and two membranous sacs of the vestibule. The axons of the cells of the vestibular nucleus form the vestibular nerve, which leaves the temporal bone through the internal auditory foramen and enters the cerebellopontine angle. The vestibular nerve enters the brain substance together with the auditory nerve into the brain at the cerebellopontine angle and ends in four vestibular nuclei (second neurons): the superior vestibular nucleus of Bechterew, the inferior vestibular nucleus of Roller, the medial vestibular nucleus of Schwalbe and the lateral vestibular nucleus of Deiters. The vestibular nuclei are located in the lateral part of the bottom of the IV ventricle - from the lower part of the pons to the middle of the medulla oblongata.
There are numerous connections of the vestibular nuclei:
The vestibular spinal tract begins from the cells of the lateral vestibular nucleus of Deiters ( tractus vestibulospinalis), which on its side, as part of the anterior cord of the spinal cord, approaches the cells of the anterior horns. Impulses carried by the vestibular nerve from the semicircular canals to Deiters' nucleus affect the spinal motor centers, especially the centers of the cervical muscles.
Bilateral connections between the vestibular nuclei and the cerebellum ( tractus vestibulocerebellaris), vestibular nuclei and reticular formation of the brain stem, as well as with the posterior (autonomic) nucleus of the vagus nerve.
The lateral vestibular nucleus of Deiters sends fibers to the medial longitudinal fasciculus ( fasciculus longius medialis) on its own and opposite sides, where these fibers take descending and ascending directions. Descending fibers descend to the spinal cord in the anterior funiculus and then switch to spinal motor neurons. The ascending fibers can be traced to the nucleus of the oculomotor nerve. The medial longitudinal fasciculus gives off collaterals to the nuclei of the III, IV and VI cranial nerves; Thanks to these connections, impulses carried from the semicircular canals to the lateral vestibular nucleus of Deiters affect the eye muscles. To carry out the function of body balance, this nucleus has connections with the proprioceptive conductors of the spinal cord.
The axons of the neurons of the vestibular nuclei transmit afferent impulses to the thalamus, the extrapyramidal system and end in the cortex of the temporal lobes of the cerebral hemispheres, presumably near the auditory projection zone.
Research methodology. By asking, they find out whether the patient has any complaints related to vestibular dysfunction: dizziness, imbalance, changes in gait, tendency to fall.
Dizziness(unpleasant false sensations of displacement in any direction of surrounding objects or the patient’s body, which intensifies when changing the position of the head, standing up and/or while walking) is one of the most common complaints when contacting a neurologist. Since patients very rarely accurately describe their dizziness, it is recommended to ask some questions when taking anamnesis. specific questions:
Under what circumstances did dizziness first occur?
What is the nature of dizziness?
Is the dizziness episodic or constant?
What is the frequency (rare, frequent) of episodes or attacks of dizziness?
What is the duration of one episode/attack (seconds, minutes, hours, days)?
In what body position does dizziness occur or worsen?
Does any change in head position (leaning down, getting into bed, turning in bed, looking up) cause dizziness?
Are there hearing problems (tinnitus, decreased hearing acuity or deafness, pressure or pain in the ear)?
Are there any visual disturbances (blurred vision, double vision, visual flashes, or floaters)?
Do sensations of rapid movements of objects that are actually stationary arise (spontaneously or with head movements)?
Does darkness or closing your eyes cause dizziness?
Is dizziness accompanied by nausea and vomiting? sweating, disorders of the cardiovascular system and breathing?
Does dizziness occur in a certain situation (in a crowd, a store, driving a vehicle, walking up stairs, etc.)?
Does the patient have associated neurological symptoms, such as swallowing problems, dysarthria, sensory disturbances in the face or trunk, and paralysis of the facial muscles and limbs?
Do you have a history of migraine attacks?
Is the patient taking any medications?
It is customary to distinguish the following types of dizziness:
Vestibular vertigo, associated with dysfunction of peripheral or central vestibular structures (inner ear, vestibular nerve, vestibular nuclei in the brain stem or their connections), is usually characterized by a sensation of rotation, often in a certain direction (right-to-left - rotational vertigo, back-to-back - linear dizziness), impaired balance and walking (vestibular ataxia) with a tendency to fall to a certain side, often accompanied by nausea, vomiting, and nystagmus. Vestibular (systemic) dizziness often occurs in the form of attacks.
· Unsystematic dizziness in the picture of a lipothymic state (manifested by a sudden onset of general weakness, a feeling of lightheadedness, “darkening in the eyes,” ringing in the ears, a feeling of “soil floating away,” a premonition of loss of consciousness, which often actually happens in the event of fainting). But the lipothymic state does not necessarily lead to fainting, it depends on the speed and extent of the fall in blood pressure. Lipotymic conditions can often recur (with orthostatic hypotension, hypoglycemic state, vasovagal variant of vegetative-vascular dystonia syndrome, etc.) and then the patient’s main complaint will be dizziness.
· A feeling of instability (shaky gait, imbalance) that occurs when walking is impaired of various origins (multisensory insufficiency; extrapyramidal, including cerebellar disorders; tumors of the posterior cranial fossa; drug intoxication).
· Psychogenic (psychophysiological) dizziness develops in patients with neurotic syndromes and personality disorders. It is often accompanied by a feeling of anxiety or fear, and often appears against the background of hyperventilation syndrome or in a certain situation (for example, when visiting a store, traveling on public transport, crossing a bridge or street, etc.). Psychogenic dizziness usually does not have a rotational nature, is associated with a feeling of instability and is often worsened by walking. Characteristic is the absence of nystagmus even at the time of severe dizziness. Many patients exhibit obsessive personality traits or depression.
Another important vestibular symptom is nystagmus(involuntary rhythmic eye movements that quickly follow each other). To identify it, the examinee’s gaze is fixed on the doctor’s hammer or finger and moved to the sides or up and down. There are two main types of nystagmus: 1) clonic(jerk-like) nystagmus, in which a slow deviation of the eyes in one direction (slow phase of nystagmus) and fast corrective movements in the opposite direction (fast phase of nystagmus) alternate; the direction of the nystagmus is determined by its fast phase; 2) less common pendulum-shaped(swing) nystagmus, which is characterized by more or less uniform deviations of the eyes in both directions, however, when looking to the side, two phases of nystagmus may appear, with the fast phase coinciding with the direction of gaze.
Nystagmus can be physiological or pathological. Thus, optical-kinetic clonic nystagmus is physiological (occurs when the gaze is fixed on moving objects, for example, on alternating black and white stripes of a rotating drum). Light symmetrical nystagmus that occurs with extreme abduction of the eyeballs is also physiological and disappears when the eyes move towards the midline. In the case when the patient observes the movement of the doctor's hammer from the maximum lateral position of the eyeballs to the opposite side by 10 degrees, and the horizontal nystagmus persists and appears asymmetrical, then they speak of pathological gaze nystagmus. Other types of nystagmus (vertical, rotatory, diagonal, spontaneous , congenital pendular, monocular, etc.) are pathological forms. In terms of amplitude, nystagmus can be small, medium or large; According to severity, nystagmus is distinguished by degree I - it occurs in extreme positions of the eyes, degree II - when looking straight, degree III - in any position of the eyes. Vestibular nystagmus occurs with angular acceleration of the head and is associated with irritation of the semicircular canals (labyrinth). In this case, irritation of the vestibular nerve and vestibular nuclei of the pons causes nystagmus in the same direction. Switching off the vestibular apparatus leads to nystagmus in the opposite direction.
To assess the state of the vestibular analyzer, statics and coordination of movements are examined at rest and while walking. When the vestibular apparatus is damaged, movements are deprived of proper regulatory movements, hence discoordination of movements (vestibular ataxia). Thus, when walking and standing, the patient tends to tilt and fall towards the affected labyrinth. If a patient in the Romberg position with his eyes closed turns his head to the left or right, he will fall towards the affected vestibular apparatus. Vestibular ataxia, unlike cerebellar ataxia, is not characterized by intention tremor. Other research methods are also used: nystagmus suppression test; vestibular nystagmus test; caloric (bithermal) vestibular test; electronystagmography, push test (Holmajai-Curthoys test); walking with eyes closed; Barani index test; Unterberger's marching test; Babinski-Weil test; otoscopy. So, when carrying out nystagmus suppression test the patient stretches his arms forward and fixes his thumbs with his gaze, then the researcher quickly turns the patient’s torso, first in one direction and then in the other. Normally, vestibular nystagmus induced by rotational movement is completely suppressed by visual fixation. The persistence of nystagmus indicates damage to the central nervous system, most often the cerebellum or its connections.
Caloric (bithermal) vestibular test– one of the most sensitive tests assessing the excitability of the labyrinths. It is carried out as follows: the patient lies down on the couch so that his torso and head are rotated 30 degrees (relative to the horizontal plane), or he sits straight on a chair, while his head is tilted back 60 degrees. When the left external auditory canal is irrigated with cold (ice) water in a volume of 5-10 ml, a healthy person experiences horizontal nystagmus directed to the right, missing to the left in the Barany index test, a tendency to fall to the left side, systemic dizziness and nausea. When the same ear is irrigated with warm water (44 degrees), nystagmus appears directed towards the irritated ear. If all these reactions are absent, this indicates that the corresponding labyrinth is not excited, or that its connections with the brain stem are interrupted. Before performing a caloric test, an otoscopy should be performed to ensure the integrity of the eardrum.
In the index Barani sample The patient, standing with his arms outstretched, is asked to place his index fingers opposite the examiner's index fingers. The patient is then asked to close his eyes and, extending his index fingers forward, touch the examiner's fingers with them. With vestibular dysfunction, there is a deviation towards the affected labyrinth.
When conducting Unterberger marching test the subject is asked to march in one place with his eyes closed, performing 40-50 steps while standing still. A healthy person remains standing in place or moves slightly relative to the starting point, or turns slightly around a vertical axis. With vestibular dysfunction, there is a deviation of the patient's torso by more than 45 degrees towards the affected labyrinth.
The results are interpreted in the same way Babinski-Weil tests(“star test”) The subject is asked to take two steps forward with eyes closed, turn around 180 degrees and take two steps back. Any deviations to the side indicate a violation (loss) of the function of one of the labyrinths. If the patient is asked to walk forward and backward several times, then as a result of deviation to one side, the trajectory of his movement may resemble the outline of a star (hence the name of the test).
Push test (Holmajai-Curthoys test) serves to study the function of the horizontal semicircular canal of the labyrinth. The researcher sharply (push) turns the seated patient's head to the side by 30-45 degrees, while the patient must fix his gaze on the tip of the researcher's nose. Thanks to the very fast vestibulo-ocular reflex, the patient's eyes remain fixed on the tip of the examiner's nose even when the head is turned. If the labyrinth function is partially or completely lost, the eyes follow the direction the head turns.
Walking with your eyes closed(in order to turn off vision control) reveals staggering to one side in a patient with vestibular dysfunction. The patient is asked to walk with his eyes closed towards the researcher for approximately 5 m. The test is repeated 3 times. With vestibular dysfunction, the patient constantly deviates towards the affected labyrinth.
A test for inducing vestibular nystagmus in a patient (in special Frenzel glasses) and a rotation test (in a special Barany chair), as well as electronystagmography, which allows quantitative assessment of the direction, speed and duration of nystagmus, are usually carried out by an otolaryngologist.
Symptoms of the lesion. In clinical practice, it is customary to distinguish between vestibular disorders of a peripheral and central nature. In this case, peripheral vestibular syndromes occur with lesions of the labyrinth, vestibular nerves and vestibular nuclei in the pons.
Labyrinthitis– diffuse or limited damage to the vestibular structures of the inner ear. Occurs in acute or more often chronic inflammation of the middle ear (with cholesteatoma), tuberculosis of the inner ear, and trauma. Labyrinthitis can be divided depending on the path of development into tympanogenic, meningogenic and hematogenous, and taking into account the inflammatory exudate - into purulent and serous. Lesions of the labyrinth usually cause a decrease in impulses from one or more semicircular canals.
In the initial stages of the disease, with acute unilateral lesions of the labyrinth, noise and hypoacusia from the affected ear, systemic dizziness, vomiting, vestibular ataxia, rotatory or horizontal nystagmus with a rapid phase towards the healthy ear occur. Nystagmus increases when the eyes are moved towards its fast phase. In the Romberg position, patients deviate towards the affected ear. With serous diffuse labyrinthitis, the phenomena of exudate and edema are determined in all parts of the labyrinth. With a favorable course of the disease, gradual resorption of exudate occurs. Limited labyrinthitis occurs with or without a fistula (usually located on the horizontal semicircular canal). With purulent diffuse labyrinthitis, persistent deafness occurs.
With labyrinthitis, as in general with peripheral damage to the vestibular analyzer of another etiology, optokinetic nystagmus is always preserved. A sign of partial damage to the vestibular function is positional nystagmus - the appearance or intensification of nystagmus when the position of the head changes.
Treatment of labyrinthitis (dehydration and anti-inflammatory medications, and, if necessary, surgical treatment) is usually carried out by an otolaryngologist.
Meniere's disease– one of the common forms of acute or chronic dysfunction of the labyrinth. Persons of both sexes most often become ill in the 4th to 6th decades of life. There are idiopathic (genetic - in 5% of patients) and symptomatic (syndrome) forms. The latter form may be a late complication of specific diseases of the labyrinth, for example, inner ear dysplasia, chronic infections of the labyrinth caused by viruses, bacteria or spirochetes with the development of autoimmune processes, as well as fractures of the pyramid of the temporal bone.
The pathogenesis of Meniere's disease is based on endolymphatic hydrops of an aresorptive or obstructive nature (“hydrops”) with a significant but uneven stretching of the membranous labyrinth, which leads to displacement of individual anatomical elements of the labyrinth, as well as to ruptures of the membranes (occurring at uneven intervals of time) separating the endolymphatic system. - and perilymphatic spaces, and to a sharp increase in the concentration of potassium in the endolymph. In this case, the function of the neurons of the vestibular ganglion of the labyrinth remains impaired until the physiological concentration of electrolytes is achieved.
An attack of Meniere's disease is characterized by: a feeling of pressure and congestion in the ear, decreased hearing, noise in the ear, severe systemic dizziness. In most patients, a feeling of fullness in the ear, a noise similar to the sound of the sea, and hypoacusia precede an attack of dizziness, gradually increase and reach its maximum at the peak intensity of the resulting rotational dizziness. Paroxysmal dizziness usually reaches such strength that it makes it impossible to maintain balance and walk, and is accompanied by significant vegetative manifestations (nausea, vomiting, sweating). Patients are forced to lie still (usually on the “healthy” side) so that the affected ear is in the highest position. During caloric and rotational tests, nystagmus is observed with a direction towards the unaffected ear. The attack passes within a few hours. At the end of the attack, as a rule, patients fall asleep, and upon waking up, they note general weakness and imbalance for several days, especially noticeable when walking. Attacks tend to recur after several weeks or months.
The course is characterized by remissions and exacerbations. At the onset of the disease, sensorineural hearing loss (mainly for low sounds) is episodic. As a result of repeated attacks, hearing steadily decreases (in some patients, even to deafness), and chronic vestibular dysfunction develops. In cases of spontaneous remissions lasting 5-10 years, the course of the disease can be considered relatively benign. In other cases, over time, the second labyrinth is also damaged: within two years - in 15% of patients, with a disease duration of more than 10-20 years - in 30-60% of cases.
For the diagnosis of Meniere's disease, in addition to the four clinical signs described above, symptoms such as unchanged perception of whispered speech and decreased perception of spoken speech, worse perception through air of a C-428 tuning fork and little changed bone conduction, lateralization of sound in Weber's experiment to a healthy ear are also important . It is important to exclude hypothyroidism, neurosyphilis, and systemic lupus erythematosus. CT and MRI are necessary only when dizziness is combined with other neurological symptoms.
The severity of an attack of Meniere's disease can be reduced or stopped with the help of antihistamines: dimenhydrinate(dramine), meclozine(bonin) at a dose of 25-50 mg every 4 hours.
The goal of treatment in the interictal period is to reduce the frequency of attacks and thereby preserve (maintain) hearing and vestibular function. For this purpose, a combination of derivatives is justified gingko biloba(Tanacan Tanacan 1 capsule 40 mg orally 3 times a day for 3 months or Ginos, in a similar dosage) with betahistine(betaserc, Betaserc, tablets 24 g, the optimal dose of the drug is 1 tablet 2 times a day after meals). Diuretics are also used (diacarb 0.25 g or hypothiazide 50 mg 2 times a day), verapamil (120-240 mg/day).
During an acute attack, reflexology (acupuncture, acupressure) is indicated, and in the interictal period, a galvanic collar according to Shcherbak with calcium chloride or pentoxifylline, reflexology, psychotherapy. In some patients, a low-salt diet is effective (no more than 1-2 g of salt per day for at least 2-3 months, and more if the effect is good). In cases of limited curability, the issue of surgical intervention is decided: in case of preserved hearing, selective transtemporal nervectomy is performed, and in case of deafness, labyrinthectomy is performed. A less invasive measure is drug inactivation of hair cells with gentamicin. Gentamicin injected as an application into the middle ear, from where it diffuses into the inner ear. At the same time, it is necessary to remember about the inevitable hearing loss.
Benign paroxysmal positional vertigo(BPPV) is one of the most common causes of vestibular vertigo in clinical practice. Occurs at any age, but more often after 60 years.
BPPV can be a consequence of traumatic brain injury, viral labyrinthitis, or damage to the labyrinth of another origin. However, in most cases it is not possible to find out the cause.
The disease is associated with the entry of particles of the otolith membrane into the posterior semicircular canal of the labyrinth. Shifting under the influence of gravity, the otoliths irritate the vestibular receptors of the dome when the head rotates in the plane of the posterior semicircular canal on the affected side and cause a paroxysm of dizziness.
The disease is characterized by short (less than a minute) attacks of intense systemic dizziness, which appear in certain positions of the head, especially when tilting it back and forth. This condition often occurs when the patient turns over in bed from his back to his side or tries to pick up an object from the floor, or get it from a high or low shelf. Dizziness is accompanied by autonomic symptoms and a feeling of discomfort. Attacks occur over several days or months. Hearing is not impaired.
To confirm the diagnosis BPPV is performed Hollike's test: The seated patient is placed on his back, while his head is lowered over the edge of the couch and turned to the side 30 degrees. In this case, the patient experiences a short-term attack of systemic vertigo, accompanied by a predominant rotatory nystagmus directed counterclockwise if the head is thrown back and to the right, or clockwise if the head is thrown back and to the left. It should be noted that nystagmus appears after a latent period lasting from one to several seconds, then its intensity quickly reaches a peak, after which it fades within 10-40 seconds. Nystagmus and dizziness are most pronounced when the patient lies on the side of the affected labyrinth. However, when placed on this side again, the intensity of these symptoms decreases. Repeated induction of an attack is possible only after a certain (quite short) refractory period of rest.
Drug therapy for BPPV is usually ineffective. To stop attacks, a special technique has been developed that allows, using positional manipulations of the head, to remove the otolith from the posterior semicircular canal, moving it to an insensitive zone (vestibule of the inner ear). To do this, the patient's head is slowly turned 180 degrees from the position causing the attack to the healthy side. There are other, more difficult to perform, positional techniques by Semon, Ellie, and others. Often, a single repositioning maneuver leads to the cessation of BPPV attacks. In resistant cases, surgical treatment is possible.
Vestibular neuritis (vestibular neuronitis)- one of the most common causes of systemic dizziness associated with damage to the vestibular nerve. The disease can occur at any age, but is more common among middle-aged people.
An infectious, probably viral etiology is suspected. Thus, often several weeks before the onset of the disease, an upper respiratory tract infection is noted, which indicates the possible viral nature of the disease. Epidemic outbreaks of this disease, which are especially susceptible to middle-aged people who do not yet have pronounced vascular risk factors in their age, also testify in favor of an infectious genesis.
The disease manifests itself as a sudden, prolonged attack of systemic dizziness with nausea, vomiting, imbalance and a feeling of fear. Symptoms worsen with any head movements or changes in body position. Patients tolerate this condition extremely hard and often do not get out of bed. Spontaneous horizontal nystagmus with a rotatory component towards the healthy ear is characteristic. During a caloric test, the reaction on the affected side is reduced or absent. There is no decrease in hearing, and audiography results remain normal. No other additional neurological symptoms were identified. Severe dizziness usually goes away spontaneously after a few hours, but may recur in the coming days or weeks. In the future, mild vestibular ataxia may persist for some time. After 1-6 weeks, all clinical symptoms regress. Most patients experience vestibular neuritis once, but sometimes, after several years, relapses occur. In the chronic form of the disease, repeated attacks of dizziness are observed without auditory impairment and other additional neurological symptoms. Attacks of dizziness are less severe, but may recur for several years.
Loss of function of the lateral semicircular canal on the affected side can be detected using a simple test: the patient is asked to fix his gaze on the bridge of the nose, then the patient's head is quickly turned to each side by 15 degrees. When turning the head to the healthy side, the gaze remains fixed. When turning the head in the direction of the lesion, the eyes shift from the point of fixation towards the direction of head movement, but then return to their original position. If no pathology is detected during this test, the diagnosis of vestibular neuritis should be questioned.
Almost any lesion of the brain stem can be accompanied by dizziness and vestibular-cerebellar ataxia (vascular vertebrobasilar insufficiency, craniovertebral anomalies, multiple sclerosis, syringobulbia, tumors of the fourth ventricle and posterior cranial fossa). In this case, the clinical manifestations of vestibular neuritis are often mistaken for a transient cerebrovascular accident in the vertebrobasilar region (TIA) or brain stem infarction. In this regard, it should be taken into account that only transient visual and oculomotor disorders that occur simultaneously, as well as dysarthria or ataxia of a mixed vestibulo-cerebellar nature against the background of systemic dizziness, and less often other neurological symptoms, indicate acute vascular ischemia in the brain stem. To suspect a TIA or infarction in the vertebrobasilar region, at least two of the symptoms listed above must be present.
Some forms of nystagmus (vertical, multiple, converging) are typical for lesions of the brain stem and are not observed with vestibular neuritis.
Attacks of Meniere's disease are manifested not only by acute vestibular dysfunction, but also by hearing loss and noise in the ear on the affected side. Combined cochleovestibular dysfunction is also observed in complicated otitis media with the development of otomastoiditis.
With tumors (acoustic neuroma, meningioma, etc.), there is a gradual increase in the intensity of systemic dizziness over a long period of time.
Specific infections (mumps, chicken pox, syphilis, tuberculosis, herpes, tick-borne borreliosis), in addition to acute vestibulopathy, are usually manifested by hearing impairment and frequent damage to other cranial nerves.
Cogan syndrome (presumably of autoimmune origin) is characterized not only by vestibular dysfunction, but also by a sharp deterioration in hearing, interstitial keratitis, and damage to the aorta.
In the acute stage, drugs against dizziness (vestibulolytic drugs) are indicated: betaserc (24 mg 2-3 times a day), scopolamine (Scopolamin 0.5 mg in the form of a patch - scopoderm or s.c.), pipolfen (Pipolfen, 25 mg every 6 hours rectally, IM or IV), Dramina (Dramina, tablet 25 mg, prescribed 25-50 mg every 6 hours rectally), Bonin (Bonin 12.5-25 mg every 12-24 hours) , Torecan (Torecan, 6.5 mg rectally or intramuscularly).
For severe nausea, medications are prescribed in suppositories or parenterally. Acupuncture and other types of reflexology can have a positive therapeutic effect.
As the condition improves, therapeutic exercises are recommended (exercises for fixing the gaze, as well as head rotation, static and then dynamic exercises for balance training, the latter include, for example, ball games).
Transverse fracture of the pyramid of the temporal bone with a brain contusion of moderate or severe severity, it is clinically characterized by complete unilateral loss of labyrinth functions with severe rotational dizziness, intense spontaneous nystagmus, vestibular ataxia, persistent deafness, damage to the facial nerve (in about half of the patients), otorhinoliquorrhea. During otoscopy, a dark color of the tympanic membrane is observed due to hemorrhage in the middle duct. In the Weber test, sound lateralizes towards the healthy ear. Patients require urgent hospitalization in the neurosurgical department.
Bruns syndrome– acute occlusion (tumor, cysticercus, etc.) at the level of the apertures of the fourth ventricle, usually occurring with a rapid turn of the head. Patients quickly develop hydrocephalic syndrome with severe headache, vomiting, vestibular dizziness and ataxia, often with forced head position, meningism, swelling of the optic nerves, respiratory and cardiovascular disorders, fainting and often death. Patients with Bruns syndrome require urgent neurosurgical care.
Central vestibulopathies occur with damage to the supranuclear vestibular connections of the brain stem and subcortical region, as well as the temporal lobe of the brain.
Brainstem encephalitis. The vestibulocerebellar form of encephalitis begins acutely with dizziness, headache and vomiting. The temperature does not always rise. Dizziness is rotational in nature with a sensation of objects spinning in a certain direction and intensifies when changing position. Less commonly, non-systemic dizziness occurs with sensations of “falling through,” “swaying walls,” and “shaking of the ground.” Balance is disturbed and patients cannot walk due to ataxia, coordination tests are performed with a miss, and they are unstable in the Romberg position. Most patients experience deviation of the arms when trying to hold a pose. Patients exhibit spontaneous nystagmus - vertical and horizontal, in one or two directions, medium or large sweeping. The disease may occur with repeated vestibular crises, but usually ends favorably. In this case, local symptoms decrease, and hyperreflexia and tonicity of experimental spontaneous nystagmus are replaced by its hyporeflexia.
It should be noted that the presence in the clinical picture of manifestations of systemic and non-systemic types of dizziness is very typical for vascular vertebrobasilar insufficiency. Vestibular dysfunction in patients with intervertebral osteochondrosis of the cervical spine, especially with posterior cervical sympathetic Bare-Lieu syndrome, can also occur as a central and/or (less commonly) peripheral (at the labyrinth level) syndrome.
Vestibular syndrome at the cortical level usually associated with damage to the temporal lobe, with experimental stimulation of which nystagmus and attacks of dizziness occur. Tumors of the temporal lobe are characterized by spontaneous attacks of dizziness with a sensation of rotation and movement of surrounding objects. Sometimes dizziness can be an aura of a temporal lobe seizure. With a tumor of the anterior parts of the temporal lobe, spontaneous small-scale nystagmus occurs, often towards the lesion. Opticokinetic nystagmus in the heterolateral direction often decreases or disappears during deep processes in the temporal lobe, which can be combined with homonymous hemianopsia and statokinetic disorders in the limbs opposite to the lesion.
Complex therapy of central vestibulopathies is carried out taking into account the etiology and pathogenesis of the disease and symptomatic remedies (including vestibulolytics), as well as physiotherapeutic procedures, reflexology, auto-training, exercise therapy and massage.
60. Due to damage to the spinal cord pathways by a pathological process, a person’s pain sensitivity in the skin and muscles is impaired. Which pathways are affected?
A. Dorsal spinocerebellar.
B. Medial spinocerebellar.
C. Ventral spinocerebellar.
D. Lateral spinothalamic.
E. Ventral spinothalamic.
61. After an injury, a patient developed a lack of movement and a violation of deep sensitivity on the right; on the left, movements are preserved, but pain and temperature sensitivity are absent. Damage to which part of the central nervous system can be assumed?
A. Motor cortex.
B. Spinal cord.
C. Midbrain.
D. Brain stem.
E. Half spinal cord injury.
62. A 35-year-old man who suffered meningoencephalitis has a sharp decrease in hearing. The examination excludes pathology of the sound-receiving and sound-reproducing apparatus of the hearing analyzer. In which gyrus of the cerebral cortex are pathological changes possible?
A. Middle temporal.
B. Corner.
C. Hippocampal.
D. Waist.
E. Greater temporal.
63. While taking state exams, a student’s pain sensitivity threshold increased. Activation of which system caused this effect?
A. Sympathoadrenal.
B. Parasympathetic.
C. Pituitary-adrenal.
D. Antinociceptive.
E. Sympathetic.
64. During a computed tomography scan, a patient was found to have a hemorrhage in the knee area of the internal capsule. Which of the following pathways will be affected first?
A. Corticonuclear.
B. Corticospinal.
C. Olive-cerebellar.
D. Tectospinal.
E. Rubrospinal.
65. In an experiment on an animal, under the action of a tactile stimulus, evoked electrical potentials arise in the cerebral cortex. Through what pathways do impulses from receptors enter the cerebral cortex?
A. Govers's Path.
B. Spinothalamic Burdacha.
E. Gaulle's spinothalamic.
66. When recording an electroencephalogram under the action of a light stimulus, evoked electrical potentials are recorded in the primary and secondary visual occipital cortex. Which of the listed structures of the central nervous system are necessarily involved in conducting excitation in this experiment?
A. Red kernels.
B. Internal geniculate bodies.
C. Upper tuberosities of the quadrigeminal.
D. Inferior tubercles of the quadrigeminal.
E. Deiters nuclei.
67. To study the activity of the spinal nerve centers in the frog, the nerve roots connecting the spinal cord with the periphery are sequentially cut. What effect is observed when all anterior roots are cut?
right side?
A. The muscle tone of the forelimbs disappears.
B. The muscle tone of the hind limbs disappears.
C. Movement of the limbs on the left side disappears.
D. Movement of the limbs on the right side disappears.
E. The “acid reflex” on the left disappears.
68. What experimental effect occurs in a frog when all dorsal roots of the spinal cord are cut on the left?
E. There are no motor disorders on the right
69. In a man with damage to one of the parts of the central nervous system, asthenia, muscle dystonia, and imbalance are observed. Which part of the central nervous system is affected?
A. Cerebellum.
B. Reticular formation.
C. Vestibular nuclei.
D. Substantia nigra.
E. Red kernels.
70. A 55-year-old patient with chronic alcoholism has impaired coordination of movement and balance as a result of damage to the structural elements of the cerebellum. Which cerebellar cells can be affected first?
A. Pear-like cells.
B. Basket cells.
C. Stellate cells.
D. Golgi cells.
E. Granule cells.
71. A victim in a car accident was diagnosed with damage to the posterior columns of the spinal cord. Which of the following dysfunctions may be associated with this injury?
A. Loss of pain sensitivity.
B. Loss of the ability to sense vibration.
C. Loss of proprioceptive and partially tactile sensitivity.
D. Loss of temperature sensitivity.
E. Increased skeletal muscle tone.
72. In a mesencephalic cat, a posture of decerebrate rigidity can be obtained. What structures need to be destroyed to do this?
A. Vestibular receptors.
B. Lateral vestibular nuclei of Deiters.
C. Red kernels.
D. Substantia nigra.
E. Quadrigeminal.
73. A decerebrate cat can be placed on the table like a doll. However, the animal cannot maintain balance (maintain an anti-gravity pose) when the surface on which it stands is tilted. This is because in a decerebrate cat:
A. There are no static vestibular postural reflexes.
B. Static neck postural reflexes are absent.
C. There are no statokinetic reflexes.
D. Static vestibular reflexes of posture are not effective enough.
E. Static neck posture reflexes are not effective enough.
74. In an experiment, a cat exhibits increased tone of the extensor muscles of the limbs and back (decerebrate rigidity). At what level was the brain section made?
A. Below the vestibular nuclei.
B. Between the spinal cord and medulla oblongata.
C. Spinal cord.
D. Below the red kernels.
E. Above the red kernels.
75. In an experiment, one of the motor structures of the brain is irritated in a cat, as a result of which an increase in the tone of the extensor muscles is observed on the stimulation side. The animal was stimulated:
A. Nucleus reticularis medialis.
B. Nukleus vestibuiaris lateralis.
C. Nucleus ruber.
D. Nukleus caudatus.
E. Nucleus intermedius Iateralis.
76. After an injury, a patient developed paralysis and tactile sensitivity disorders on the right; on the left there is no paralysis, but pain and temperature sensitivity is impaired. What is the reason for this phenomenon?
A. Damage to the motor zone of the cerebral cortex.
B. Unilateral spinal cord injury on the right side.
C. Damage to the brain stem.
D. Damage to the cerebellum.
E. Damage to the midbrain.
77. At the start of a competition, an athlete experiences an increase in blood pressure and heart rate. The influence of which parts of the central nervous system can explain these changes?
A. Cortex of the cerebral hemispheres.
B. Medulla oblongata.
C. Midbrain.
D. Diencephalon.
E. Hypothalamus.
78. A 33-year-old man was diagnosed with perforation of the stomach and inflammation of the peritoneum, which led to tension in the muscles of the anterior abdominal wall (“board abdomen”). What reflex provides this symptom?
A. Somato-visceral.
B. Viscero-visceral.
C. Cutanovisceral.
D. Viscero-somatic.
E. Viscero-cutaneous.
79. In a sick person, hemorrhage in the posterior central gyrus led to impaired sensitivity on the opposite side. What type of sensitivity is impaired?
A. Cutaneous and proprioceptive.
B. Auditory and visual.
C. Olfactory and gustatory.
D. Auditory.
E. Visual.
80. The four-tubercle structure was destroyed in a mesencephalic cat. What reflexes will disappear as a result of this?
A. Straightening the head.
B. Straightening the torso.
C. Primary indicative.
D. Stato-kinetic when moving with angular acceleration.
E. Stato-kinetic when moving with linear acceleration.
81. An electromyographic examination found that when the flexors are excited, the tone of the extensors simultaneously increases. What principle of interaction between nerve centers is partially broken?
A. Dominant.
B. Feedback.
C. Occlusion.
D. Relief.
E. Reciprocal inhibition.
82 . An experiment is carried out on a spinal frog. After increasing the area of skin affected by the acid solution, the time of the protective flexion reflex decreases from 10 to 6 seconds. Which of the following mechanisms underlies the reduction in reflex time?
A. Excitation recirculation.
B. Temporal summation of excitation.
C. Spatial summation of excitation.
D. Irradiation of excitation by divergent nerve circuits.
E. The principle of dominance.
83. The histological specimen shows an organ of the nervous system that has gray and white matter. Gray matter is located on the periphery. The neurons in it form three layers: molecular, ganglionic and granular. To which organ do these morphological characteristics belong?
A. Cerebral cortex.
B. Spinal cord.
C. Medulla oblongata.
D. Bridge.
E. Cerebellum.
84. A 60-year-old man experienced prolonged sleep after a cerebral hemorrhage. Damage to which structures most likely led to this condition?
A. Reticular formation.
B. Substantia nigra.
C. Cerebral cortex.
D. Hippocampus.
E. Nuclei of cranial nerves.
85. A 70-year-old patient has been diagnosed with hemorrhage in the brainstem. The examination revealed an increase in the tone of the flexor muscles against the background of a decrease in the tone of the extensor muscles. Irritation of what brain structures can explain the changes in muscle tone in this case?
A. Quadrigeminal.
B. Reticular formation.
C. Vestibular nuclei.
D. Red kernels.
E. Substantia nigra.
86. In a person with damage to one of the parts of the central nervous system, the following were observed: asthenia, muscular dystonia, imbalance. Which part of the central nervous system can be damaged in this case?
A. Cerebellum.
B. Substantia nigra.
C. Reticular formation.
D. Red nucleus.
E. Cochlear nucleus.
87. A 32-year-old man is in a state of stress due to an industrial conflict. What hormone triggered the body's stress response?
A. Adrenaline.
B. Thyrocalcitonin.
C. Parathyroid hormone.
D. Testosterone.
E. Melanotropin.
88. After strychnine is injected into a frog, it responds to minimal stimulation with generalized convulsions. Blockade of which central nervous system structure causes this?
A. Cholinergic receptors.
B. Adrenoreceptors.
C. Excitatory synapses.
D. Inhibitory synapses.
E. Renshaw cells.
89. A 50-year-old man who suffers from chronic alcoholism was given an injection of chlorpromazine into a vein to relieve aggression and delirium. The patient lost his memory. What is the most likely cause of the complication that has arisen?
A. Blockade of the Russian Federation.
B. Violation of coronary circulation.
C. Orthostatic collapse.
D. Imbalance of oxidative processes in the brain.
E. Inhibition of the limbic system.
89. The γ-loop plays an important role in the formation of decerebrate rigidity. This is confirmed experimentally, since the degree of rigidity decreases significantly after destruction of the following structures of the spinal cord:
A. Lateral horns.
B. Dorsal roots.
C. Posterior horns.
D. Anterior roots.
E. Anterior horns.
90. A study on the spinal frog found that an increase in the surface area of the skin of the limb, which is exposed to a solution of 0.3% HCl, leads to a decrease in the time of the protective flexion reflex and to an increase in the intensity of the reflex response. A change in reflex time and intensity of the reflex response is the result:
A. Irradiation of excitation to the central nervous system.
B. Convergence of excitation in the central nervous system.
C. Simultaneous summation.
D. Sequential summation.
E. Recirculation of excitation to the central nervous system.
91. At the start of a competition, an athlete experiences an increase in blood pressure and heart rate. The influence of which parts of the central nervous system can explain these changes?
A. Midbrain.
B. Cerebral cortex.
C. Hypothalamus.
D. Medulla oblongata.
E. Diencephalon.
92. After a hemorrhage in the area of the thalamus, the patient noticed that he did not feel pain from a needle prick during intramuscular and intravenous injections. Which nuclei can be assumed to be affected?
A. Ventrolateral nuclei of the thalamus.
B. Medial geniculate bodies.
C. Lateral geniculate bodies.
D. Associative nuclei.
E. Red kernels.
93. When pushing a barbell, the athlete throws his head back to maximize the tone of the extensor muscles of the upper limbs. Where are the centers of the reflexes that arise in this case located?
A. In red nuclei.
B. In the spinal cord.
C. In Deiters' nuclei.
D. In the basal ganglia.
E. In the motor cortex.
94. A 36-year-old patient, after a road injury, developed paralysis of the muscles of the limbs on the right, loss of pain and temperature sensitivity on the left, and a partial decrease in tactile sensitivity on both sides. For damage to which part of the brain will these changes be most characteristic?
A. The right half of the spinal cord.
B. Posterior columns of the spinal cord.
C. Motor cortex on the left.
D. Left half of the spinal cord.
E. Anterior columns of the spinal cord.
95. After a work injury, the victim was taken to the hospital with a spinal injury. A lesion was detected in the posterior cords of the spinal cord at the level of the 1st thoracic vertebra. What pathways were affected in this case?
A. Pain and temperature sensitivity.
B. Corticospinal.
C. Spinocerebellar.
D. Tactile and proprioceptive sensitivity.
E. Extrapyramidal.
96. After a car accident, a man had an X-ray examination of a displaced spinal injury at the level of I - II thoracic segments. Neurologically, a violation of motor function and loss of deep sensitivity on the right and loss of superficial sensitivity on the left are determined. What possible variant of spinal cord injury is possible for the patient?
A. Brown-Séquard syndrome.
B. Central paralysis.
C. Damage to the anterior horns of the spinal cord.
D. Damage to the pyramidal tract.
E. Total spinal cord injury.
97. A patient has a significant decrease in the knee reflex. What segments of the spinal cord are damaged?
A. III-IV lumbar.
B. I-II sacral.
C. VII -VIII thoracic.
D. V-VI cervical.
E. IX-X chest.
98. After a plane crash, a man was admitted to the hospital with severe injuries to the pelvic bones, lower and upper extremities, and skull. During the first week he did not wake up. What could be the cause of prolonged sleep?
A. Painful shock.
B. Deficiency of excitatory neurotransmission.
C. Rupture of the ascending reticular formation.
D. Damage to the bones of the skull.
E. Damage to the cerebellum.
99. In an experiment, the anterior roots of five segments of the spinal cord were cut in an animal. What changes will occur in the innervation zone?
A. Loss of tactile sensitivity.
B. Loss of temperature sensitivity.
C. Hypersensitivity.
D. Loss of proprioceptive sensitivity.
E. Loss of movement.
100. The patient gets tired quickly when working. When standing with his eyes closed, he staggers and loses his balance. Skeletal muscle tone is reduced. Which of the following brain structures is most likely affected in this person?
A. Basal ganglia.
B. Limbic system.
C. Cerebellum.
D. Precentral gyrus of the cerebral cortex.
E. Thalamus.
101. Due to the growth of a tumor into the cavity of the third ventricle of the brain, the patient develops autonomic disorders in the form of sleep disorders, thermoregulation, all types of metabolism, and diabetes insipidus. Irritation of the nuclei of which area of the brain causes these symptoms?
A. Hypothalamus.
B. Midbrain tegmentum.
C. Brain peduncles.
E. Medulla oblongata.
102. A 60-year-old man has been diagnosed with a stroke in the region of the lateral nuclei of the hypothalamus. What behavioral changes should we expect?
A. Refusal to eat.
B. Aggressiveness.
C. Depression.
E. Gluttony.
103. A patient complains of pain in his amputated leg. What is the most likely mechanism for this phenomenon?
A. Decreased tone of the endogenous opiate system.
B. Increased stimulation of central (adrenoreactive) structures.
C. Violation of gate control.
D. Formation of a neuroma in the nerve stump.
E. Hypersensitivity of neurons of the nociceptive system.
104. After a domestic injury in a patient. At the age of 18, constant dizziness, eye nystagmus, chanted speech, and uncertain gait appeared. This indicates a dysfunction:
A. Substantia nigra.
B. Motor cortex.
C. Vestibular nuclei.
D. Basal ganglia.
E. Cerebellum.
105. During physical activity, a person is less sensitive to pain. Activation of which structure causes this?
A. Adrenal glands.
B. Antinociceptive system.
C. Sympathoadrenal system.
D. Nociceptive system.
E. Thyroid gland.
106. Due to the destruction of certain structures of the brain stem, the animal lost its orientation reflexes. What structures were destroyed?
A. Medial nuclei of the reticular formation.
B. Vestibular nuclei.
C. Red kernels.
D. Substantia nigra.
E. Quadruple.
107. A 33-year-old man has impaired pain and temperature sensitivity due to a spinal cord injury, which is caused by damage to the following ascending pathways:
A. Spinocortical Burdacha.
B. Spinothalamic.
C. Dorsal spinocerebellar.
D. Spinocortical Gaulle.
E. Ventral spinocerebellar.
108. A pathological examination of the spinal cord of a 70-year-old man revealed destruction and a decrease in the number of nuclei of the anterior horns in the cervical and thoracic regions. What functions were impaired during life?
A. Sensitivity and motor functions of the upper limbs.
B. Motor functions of the lower extremities.
C. Sensitivity of the upper extremities.
D. Motor functions of the upper limbs.
E. Sensitivity of the lower extremities.
109. In an experiment on an animal, under the action of a tactile stimulus, evoked electrical potentials arise in the cerebral cortex. Through what pathways do impulses from receptors enter the cerebral cortex?
A. Govers's Path.
B. Spinothalamic Burdacha.
C. Spinothalamic ventral.
D. Spinothalamic lateral.
E. Gaulle's spinothalamic.
110. What experimental effect occurs in a frog when all dorsal roots of the spinal cord are cut on the left?
A. Movement of the limbs on the left disappears.
B. Movement of the limbs on the right disappears.
C. The flexor tone of the muscles on the left disappears.
D. The flexor tone of the muscles on the right disappears.
The vestibular nuclei complex turned out to be much more complex than the “ordinary cranial nerve nucleus.”
- This is not the only purpose of vestibular afferents: the cerebellum also receives them.
- Most of the neurons of the vestibular nuclei, on the contrary, do not receive such afferents, but receive proprioceptive and visual information
- The largest entrance to the complex is generally from the cerebellum (Vidal, Sans)
- Classical nuclear boundaries are highly controversial
Anatomy of the nuclei of the vestibular complex
Neal Barcmack. Vestibular Nuclei and Their Cerebellar Connections. 2015. See transcript in text
Classically, histologists distinguish four nuclei, based on the morphology of the cells - but we must remember (I refer to this many times throughout these notes) that there are no clear boundaries between these nuclei, there are “territorial” disputes between different authors regarding their boundaries, and the well-established nuclear fission probably has little to do with their function.
- SVN - Superior Vestibular Nucleus, or Bechterew’s nucleus (he himself called it angular nucleus). The only nucleus characterized by a relatively uniform distribution of medium-sized neurons.
- LVN - Lateral Vestibular Nucleus, also Deiter's nucleus - characterized by its huge cells, which, however, are concentrated in the dorso-caudal part, which gives rise to disputes regarding the boundaries of this nucleus. In the rostro-ventral part, neurons are more standard in size, and the boundaries with the SVN are in the rostro-ventral part. the dorsal part is difficult to distinguish. The boundaries with the DVN are also controversial, and the DVN also contains giant cells. Some sources call LVN only what contains huge cells. The confusion with this particular nucleus is enormous: most sources follow Brodal and Pompeiano, while simultaneously believing that they captured a piece of the magnocellular MVN.
- DVN - Descending Vestibular Nucleus, or IVN - Inferior VN, or even spinal vestibular nucleus. There is a "territorial dispute" in the sources between DVN and LVN. It was called spinal at a time when it was believed that the vestibular nerve had a spinal branch, and this nucleus served as its root.
- MVN - Medial Vesibular Nucleus, or Schwalbe's nucleus. Previously, it was also called triangular - nucleus triangularis, and even principal vestibular nucleus. Probably the largest of the vestibular nuclei. There is a "territorial dispute" in the sources between MVN and LVN. In this nucleus (it is the largest in size) there are neurons of various sizes. Sources also differ about their size gradient - some write about a dorsal cluster of small (parvocellular) cells and a ventral cluster of larger (magnocellular) neurons, others say that the gradient is actually caudal-rostral. The rostral part of the MVN contains VOR neurons (presumably magnocellular), while the caudal part contains regulators of autonomic functions, parvocellular. Brodal also identified a cluster “m” of especially large cells in it, but did not establish the function at all.
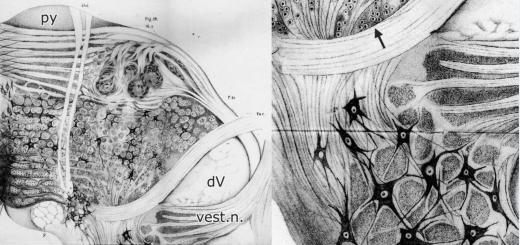
The picture shows the kernels in three sections (C is just an enlarged B)
Other nuclei with clear connections to the vestibular system
- The Psol - parasolitary nucleus - also receives vestibular projections, and many consider it the “fifth” nucleus. Mainly routes outgoing communications to Inferior Olive
- Complexes X, Y and Z. They do not receive direct vestibular projection, but are apparently integrators of proprioceptive information. Particularly characteristic here is complex X, which is confidently highlighted in works on somatosensory-vestibular integration, and complex Y, which serves as a source of vestibulo-thalamo-cortical pathways
- NPH - nucleus prepositus hypoglossi, which has functionally similar connections with the vestibulocerebellum and similar projections - and although a certain number of direct inputs of the vestibular nerve also fall there, it receives its main input from the “real” vestibular nuclei (Büttner-Ennever). It is considered a source of information ascending to the cortex primarily for head direction cells
- The NRGc nucleus reticularis gigantocellularis is the nucleus of the reticular formation, and although it is especially important for vestibular/postural function, virtually all of the surrounding reticular nuclei are connected to it in one way or another, and are the source of the reticulospinal tract
Other designations: Ecu external cuneate nucleus, Flflocculus, icp inferior cerebellar peduncle, IO inferior olive, Nsol solitary nucleus, Pyramidal tract, SO superior olive; SpV spinal trigeminal nucleus, 7 facial nucleus
Morphology using the example of Lateral Vestibular Nucleus

A luxurious, bomb drawing from the work of Otto Deiters himself, after whom the Deiters nucleus is named Lateral Vestibular Nucleus. Publication of 1865 (!), apparently drawn earlier, since Deiters died of typhus in 1863, at the age of only 29 years. Just think about it - this is drawn before the Cajal and the Golgi and the debate about what a neuron is. Absolutely amazing work. Deiters used his own staining technique (the Golgi reaction was still 10+ years away). Abbreviations (added later during re-publication): dV descending trigeminal root, py pyramid, rest.b. restiform body - also known as the inferior cerebellar peduncle, vest.n. vestibular nerve (in fact, Deiters, as was common in his time, called it the “acoustic nerve”). The “reticular formation” is clearly visible in the center of the trunk. Although Deiters himself was not a supporter of the reticular theory of the nervous system, these drawings of his were actively used by its supporters.
I present this picture (besides the fact that this is the brightest piece of history that should not be forgotten) as an illustration of the morphological characteristics by which histologists identified nuclei. These huge black neurons - giant Deiters cells - are considered a characteristic feature of the LVN. Although this is not the only class of neurons in it, of course. There are also medium-sized and small neurons, which, however, are morphologically quite similar to giant ones.
However, the presence of neurons of such different sizes hints at multiple (top-down?) systems within this nucleus. This has led to controversy from Deiters' time to the present day. Deiters, for example, denied the existence of a connection from the vestibular nerve to the nucleus of his name. Those who followed explored it; on the contrary, they found it. Even more careful subsequent researchers noted that there are connections, but they avoid precisely the giant Deuterus cells, so both Deuters and everyone else are right. Go figure it out.
Inputs to the vestibular nuclei

Projections of the vestibular nerve according to Barmack 2003. On the right picture are projections of the semicircular canals into the vestibular nuclei. Notice how they bypass the lateral vestibular nucleus
The axons of the primary vestibular neurons of Scarpa's ganglion bifurcate at the entrance to the trunk, and a smaller part goes to the cerebellum, the majority to the vestibular nuclei. The boundaries of the vestibular nuclei, determined by histologists, are “not respected”; the topography of the projections of afferents almost does not intersect with the boundaries of the vestibular nuclei. Almost the only, and negative topographical exception is that there are projections from the horizontal canal to all nuclei, except Lateral Vestibular Nucleus.
Hair cells and their corresponding neurons in Scarpa's ganglion are divided into two classes - regular and irregular. Despite the fact that this division is being actively studied, their functional role is still unclear, and therefore I will not dwell on them in detail here (more details see Cullen 2012)

Inputs to neurons of the vestibular nuclei from the point of view of pharmacologists Soto et al: Neuropharmacological basis of vestibular system disorder treatment 2013
Correct interpretation of primary signals requires a combination of, for example, signals from the otoliths and semicircular canals (individually this is inconsistent). Therefore, we tested the hypothesis about the presence of second-order vestibular neurons (in the nuclei) that simultaneously receive monosynaptic input from canals and otoliths, or from different canals. - Vestibular convergence. Such neurons exist, but are rare. However, many neurons in the vestibular nuclei (if not most) receive indirect convergent information through polysynaptic pathways. (McCrea et al 2006)
Vestibular afferents are only one of the input signals from the vestibular nuclei. Most neurons of the vestibular nuclei receive the same: (Barmack 2005)
- Visual inputs - see Additional Visual System
- From the spinal cord in different ways, see Somatosensory-vestibular_integration
- Inputs from the cerebellum (mainly, but by no means only, the vestibulocerebellum). The vestibulocerebellum works directly with the vestibular nuclei, the remaining sections work through the deep cerebellar nuclei. This aspect is sometimes expressed in the statement that "the vestibular nuclei are the deep nucleus of the vestibulocerebellum"
- From the motor cortex - these connections are thought to be particularly strong on vestibulospinal neurons
In addition to these inputs, special mention should be made of the Vestibular corollary discharge
Outputs from the vestibular nuclei, see separate articles Vestibulospinal tracts Vestibular cortex
Classification of neurons of the vestibular nuclei

Figure 1.5 from Büttner-Ennever
Neurons of the vestibular nuclei can be divided into projection (sending axons outside the system), commissural (sending axons to the vestibular nuclei on the other side, not necessarily of the same name), and non-projection. Projection neurons can simultaneously be second-order neurons, i.e. receive direct input from first-order neurons from Scarpa's ganglion, and in this case they form the three-neuron circuit beloved by all textbooks, for example VOR. However, there are also projection neurons that do not receive vestibular inputs. (Figure 1.5 shows the projection neurons of the oculomotor nuclei, shaded areas - neurons without direct vestibular inputs. Points and triangles - second-order projection neurons having vertical sensitivity, circles - horizontal (presumably from the corresponding semicircular canals)). Again, I note that in this map the analogue of somatotopy is very poorly visible, and certainly all poor compliance with the boundaries of the vestibular nuclei.
Second-order projection neurons have the following common classification, derived mainly from studies of the vestibulo-ocular reflex (see articles by Cullen), and therefore have a strong bias there, but due to their active use in the literature, it needs to be described.
- PVP - Position-vesibular-pause neurons. They are so called because their activity stops during eye saccades. These are the main VOR neurons, the majority of them
- EH - Eye-head neurons, also FTN - floccular target neurons, these are also VOR neurons, characterized by input from the cerebellum (flocculus) and presumably providing VOR adaptation
- VO - Vesibular only - do not participate in oculomotor circuits, presumably build vestibulospinal reflexes and projections to the cortex, including for assessing one’s own movement. They have mutual connections with the nodulus/uvula of the cerebellum. In modern literature, the name “Vestibular only” is considered unsuccessful, and they are called Non-Eye-Movement neurons - NEM. (McCrea)
To date, there is no evidence of how complete this classification is outside of oculomotor studies. In particular, it is reliably known that there are neurons of the vestibular nuclei that simultaneously project both the oculomotor nuclei and the spinal cord - their axon bifurcates and goes both up and down - Fig. 1.7 from Büttner-Ennever, 1.3.2.3.
In this regard, it is not clear how to relate to Cullen’s statements about the absence of optokinetic inputs for VO neurons - until a complete map of the neurons of the vestibular nuclei has been built, it is almost impossible to draw such conclusions (optokinetic effects on both putative functions of VO neurons are clearly demonstrated).
The described classification is not the only one. For example, the Uchino group (for more details, see Vestibulospinal tracts) offers a classification - VO - vestibulo-oculomotor, VC - vestibulocervical, VOC - both cervical and oculomotor, VS - vestibulospinal.
Note that VO here and in the previous diagram mean exactly the opposite, so the classifiers need an eye and an eye.
Commissural tracts

from the works of Goldberg, zones of projection neurons are highlighted in color, black arrows - commissural pathways, empty - intranuclear (intrinsic)
Correct interpretation of vestibular signals is impossible without comparing data from the left and right labyrinths. This comparison is provided by the commissural pathways crossing the midline. The classic picture of a system of such connections is shown in the figure on the right.
A few observations commonly cited in the literature regarding this system:
- Commissural connections reliably link the NPH with the vestibular nuclei - although the NPH does not receive direct input from the vestibular nerve, it actively projects to the opposite vestibular nuclei
- The LVN does not send commissural connections.
- In fact, this statement can be carefully expanded - in the figure on the right, the location zones are highlighted in color projection neurons of the vestibular nuclei, which are the source of oculomotor and spinal projections (see diagram above too). They do not make commissural projections
- Once again, I note that the spinal projection zone confidently lies at the intersection of the classical boundaries of the nuclei
- This system can give another classification of neurons of the vestibular nuclei (these sets intersect)
- secondary neurons receiving direct projections from the vestibular nerve (primary ones are all in Scarpa's ganglion according to established nomenclature)
- projection neurons sending axons to oculomotor or spinal motor or autonomic centers (some of these are secondary inputs, especially true for SVN-VOR neurons)
- commissural neurons (they probably cannot be projection neurons)
- internal, intrinsic neurons that provide connections between the nuclei of the complex, but do not cross the midline. Probably a significant part of them are FTN - floccular target neurons, see above
Functions of the vestibular nuclei

McCall&Yates 2011
The classic four vestibular nuclei are present in all mammals. In birds, histologists distinguish six nuclei; in reptiles there may be fewer, but the functional role of the vestibular complex is distributed among the nuclei not in accordance with histological boundaries.
Attempts to determine the functions of each kernel individually are however quite unsuccessful, and I like a different approach
Figure 4 from the McCall&Yates article shows the supposed functional specialization of the vestibular complex in cats, where Cognition refers to participation in spatial navigation (vestibular input to hippocampal place cells, etc.). This horizontal division corresponds quite well to the division into embryological zones - rhombomeres, see Straka et al 2014, and in this classification (hodological mosaic) the vestibular complex is quite conservative between birds, mammals and reptiles and even amphibians (data, however, are still quite small)
The picture of functional roles somewhat contradicts Fig. 1.5. from the previous section, but in this science everything is like that.
The autonomic control referred to here is the regulation of blood pressure, which requires a sufficiently rapid response in response to changes in body position to ensure adequate performance. These changes in vascular tone are dealt with by the autonomic nervous system, which receives input from the corresponding sections of the vestibular nuclei.
A second possible connection to the autonomic nervous system is somatic gravitception.
An important conclusion: the functions of the vestibular nuclei are incongruent with their boundaries. In particular, the identification of LVST neurons by modern methods shows that it does not coincide with the boundaries of the LVN in any way.
Somatotopy LVN

LVN, Brodal 1974, Fig. 15. In his diagram, the cervical and lumbar projecting neurons are clearly separated. There is somatotopy. Modern works (see below) do not confirm this

Basaldella, Arber 2015. In the upper part, all spinal-projecting neurons are marked; those that are within the Lateral Vestibular Nucleus are highlighted in color (the rest are in the DVE, which the authors call spinal. In the lower part, only those that form monosynaptic projections to motoneurons are marked. Please note that in the dorsal part of the VLE there are no monosynaptic projections to motor neurons at all, and in the ventral part, although the “gradient” of Brodal somatotopy is more or less preserved, everything is too mixed up to talk about somatotopy
Brodal identifies somatotopy in the Lateral Vestibular Nucleus, corresponding to the somatotopy of the vestibulospinal tract emanating from it. The figure on the right shows a projection organization diagram; I note that this is a view from the lateral side, i.e. The core is rotated 90 degrees relative to the other diagrams on this page.
Somatotopy of the LVN is a controversial story, since more recent studies have shown that the vestibulospinal tracts actively branch, innervating many segments of the spinal cord with one neuron, but at least grouping into cervical and lumbar neurons is generally observed (Boyle)
The somatotopy of the LVN is also controversial for the reason that it assumes (many authors follow this implicit assumption) that this nucleus is entirely the source of the vestibulospinal tract, and the exit zone of the corresponding axons of the tract corresponds to the role of the nucleus itself.

In the drawing, cynically redone by Jan Vogt of Brodal & Pompeiano, their drawings of the LVN superimpose another division of the nucleus - into the ventral part, which receives direct projections from the vestibular nerve, and the dorsal part, which is actively controlled by the cerebellum ("zone B") and contains giant Deiters neurons. If we combine these ideas, it turns out that the area of the hind legs (drawing and diagrams about cats) is controlled by the cerebellum, and the area of the neck and possibly the front legs is controlled directly by the vestibular nerve.
Brodal writes that the size of Deiters' giant cells corresponds to somatotopy: the larger cells (perhaps? this is just an assumption on his part) correspond to the thicker fibers in the tract going to the lumbar regions, and this explains their size. This hypothesis appears to be wrong
- The organization of precisely LVN projections into motor neurons, in their monosynaptic part (presumably just giant cells) is different for the hind and forelimbs, even in cats, which are tetrapods (see Anti-gravity tone). But the functionality of this projection has not been reliably established. Two hypotheses are interesting
- Fall response (often expressed by the Grillner group because they found a high motor neuron firing threshold)
- Recent evidence in the article by Basaldello, Arber 2015, where the authors found a preferential connection of monosynaptic projections to slow motor neurons, from which it can be concluded that vestibulospinal innervation maintains anti-gravity tone
- The neck is indeed controlled by the vestibular system in a completely different way than the axial muscles of the back and especially the limbs, and there are indeed functional monosynaptic reflexes there
- The diffuse distribution of giant cells hints that there may be at least two systems within the LVN, with different functions (as in the striatum for example)
However, I will reiterate the point that the functions of the vestibular nuclei and especially the LVN are incongruent with their boundaries. This concept was not accepted at all in the 60-70 years, when Brodal, Lund and others performed studies on the basis of which the conclusion was made about somatotopy in the LVN. The method of stimulation with the LVN electrode does not have sufficient resolving accuracy, so the statement about somatotopy in the LVN should be considered controversial - but has not yet been clearly refuted by higher-resolution studies.
conclusions
Over the course of decades, a clear answer to the question of what the “real” boundaries of the vestibular nuclei are has not been formed in the literature. These discrepancies easily lead to different conclusions: For some, destruction of the LVN clearly leads to the disappearance of decerebrate rigidity, for others it does not (Magoun 1949). Some write that the LVN does not receive direct vestibular inputs, others that it is the opposite. For some, the LVN and the source of the LVST tract are identically the same thing, and they look for somatotopy in it (Brodal), for others the LVST turns out to come out of the DVN, and even a little from the MVN. It becomes impossible to unambiguously understand the results of many works that follow some kind of kernel boundaries, such as Uemura & Cohen 1974, since the boundaries of the kernel and the boundaries of the function do not coincide.
Most likely, the attempt to understand the vestibular system as a set of morphologically defined nuclei with a homogeneous function is a dead end. Even an attempt to divide them into “magno-parvocellular” parts does not yield results. The vestibular system is apparently closer in structure to the reticular formation with which they have extremely much in common. The territory of the nuclei is occupied by neurons of different functions, which are probably well mixed among themselves.
To understand the functions of the vestibular complex, it is necessary to use tools with resolution at the level of individual neurons: immunohistochemical, embryological, optogenetic. So far there are few of them, but individual works appear - see Straka 2014 or Maria di Bonito 2015. In these works, starting from rhombomeres- temporary divisions of the rhombencephalon, which are “marked” during embryonic development by HOX genes - it is possible to detect a fairly clear functional division of groups of neurons according to their origin.
In particular, it was possible to almost unambiguously link all LVST source neurons to a specific group of neurons originating from rhombomere r4(the territory of the Hoxb1 gene, on the basis of which they are marked). During the process of embryogenesis in some species they then “climb” into the territory of r3 and r5, but in the initial stages the border is clear! This allows (see the argumentation in the work of Di Bonito) to define the LVST group - the source of the lateral vestibulospinal tract - as a single functional group of neurons.
In this case, the LVST group partially “climbs” into the territory of the neighboring nuclei - DVN and MVN, and the source groups of vestibulo-ocular projections and MVST projections appear on the territory of the LVN.
The statement "all LVST neurons come from r4" does not mean that r4 only gives rise to LVST - it is in fact the most ancient segment of the vestibular organization, it is in r4 that the vestibular nerve enters, and therefore it gives rise to many other classes of neurons (see diagram), including efferent, for example.
The approach of labeling neuronal groups in the vestibular system in this way offers hope. But questions remain - in such a “genetic excision” of the LVST, mice come out surprisingly functional, retaining all the functions traditionally attributed to this tract (they even eventually restored the vestibulospinal reflex, after a period of its almost complete absence), and bringing to the fore rather unconventional ones vestibular complex, functions not related to balance and tone - such as, for example, loss of stable alternation of limbs during locomotion.
Literature
The place where the first one ends vestibular nerve neuron are four nuclei located under the bottom of the 4th ventricle. The first nucleus, called Deiters' nucleus, is located in the lateral part of the medulla oblongata and consists of very large motor-type cells. The triangular nucleus lies closer to the midline of the rhomboid fossa. Bekhterev's nucleus is located in the lateral angle of the 4th ventricle. Like the spinal dorsal roots and other sensory cranial nerves, the vestibular nerve sends down fibers that make up the spinal vestibular root and end in the cells accompanying the named root. The collection of these cells is called the Rolleroo nucleus.
Klosovsky, in addition, he isolated a cellular formation in humans and animals located in the vestibular nerve itself. He called it the intraradicular nucleus of the vestibular nerve.
From cells of the vestibular nuclei ascending and descending fibers originate. The system of descending fibers arises primarily in the cells of Deiters' nucleus and constitutes the lateral vestibulospinal tract, which ends in the motor cells of the anterior horns of the spinal cord, innervating the muscles of the trunk and limbs. The descending system includes fibers coming from the cells of the triangular and roller nuclei. Fibers from the cells of these two nuclei descend as part of the posterior longitudinal fasciculus and end mainly in the anterior horns of the cervical part of the spinal cord.
Ascending fiber system consists of straight, uncrossed fibers arising from cells and ascending as part of the posterior longitudinal fasciculus to the nuclei of the oculomotor nerves and the nuclei of the bottom of the Sylvian aqueduct. The triangular nucleus and, possibly, part of the Roller nucleus give rise to intersecting fibers, which also rise as part of the posterior longitudinal fasciculus to the oculomotor nuclei and the nuclei of the bottom of the Sylvian aqueduct. In addition, it is necessary to note the presence of fibers arising in the ankylosing spondylitis nucleus and heading to the reticular substance of the medulla oblongata and ending in the latter. However, the bulk of the fibers going to the vegetative centers in the reticular substance of the medulla oblongata comes from the triangular nucleus.
Vestibular apparatus functions predominantly reflexively. At the same time, it should be taken into account that in humans, when the vestibular apparatus is irritated, conscious sensations arise: a sensation of linear and rotational movement in space, and in pathological cases, various types of dizziness. In other words, there is an anatomically not yet specified vestibulocortical reflex arc. Evidence of the existence of such a path will be provided by studying the electroencephalogram during stimulation of the labyrinth. During the rotation test in cats, an increase in the cortical electrical potential was found, and this effect did not exist after removal of the labyrinths. An increase in potential is noted in certain areas of the cortex of the temporal and frontal lobes. These experiments speak in favor of the existence of a projection of the vestibular apparatus into the cortex of the temporal lobe (adjacent to the parietal lobe) and into the cortex of the frontal lobe. A caloric test in monkeys revealed a change in potential in the frontal cortex.
After strychninization Thus found in the vestibular zones in the temporal and frontal lobes of cats and dogs, it was possible to obtain a seizure of reflex epilepsy after labyrinthine stimulation, which is explained by the spread of excitation from these strychnine-sensitized zones to the motor cortex of the brain.
III-nucleus of the oculomotor nerve, IV-nucleus of the trochlear nerve, VI-nucleus of the abducens nerve, D - Deiters' nucleus. T - triangular nucleus, N.K. - nucleus of the descending root, B - ankylosing spondylitis nucleus, P - tegmental (roofing) nucleus of the cerebellum, 3. P.P. - posterior longitudinal fasciculus, B.P. - lateral lemniscus, S.V - Sylvian aqueduct. D. A. - Darkshevich nucleus, I - interstitial nucleus, K, I. - red nucleus, 3. B. - optic thalamus, B. Sh. - globus pallidus, K. - cerebral cortex, 1 - crossed vestibulo-mesencephalic fascicle horizontal vestibular tract, 2 - direct vestibulo-mesencephalic fascicle of the frontal vestibular tract, 3 - direct vestibulo-mesencephalic fascicle of the sagittal vestibular tract, 4 - ascending branch of the vestibular nerve, 5 - descending branch of the vestibular nerve, 6 - vestibulo-spinal fascicle, 7 - connections between the vestibular nuclei for mutual inhibitionIn favor the existence of such a vestibular-cortical pathway suggests the possibility of conditioned reflexes in dogs in response to angular acceleration and even their recognition of the direction of such acceleration. Thus, I. P. Pavlov’s teaching on conditioned reflexes sheds new light on the issue of vestibular representation in the cerebral cortex.
More detailed study posterior longitudinal fasciculus indicates the presence of ascending fibers from various vestibular nuclei. On the one hand, the posterior longitudinal fasciculus includes fibers originating from the cells of the triangular and, possibly, Rollerian nuclei. At the level of the location of the nuclei of the VI pair of nerves, the fibers move to the opposite side and rise to the nuclei of the IV and III nerves, on the cells of which they end. Part of the fibers of this path goes further to the Darkshevich nucleus and to the optic thalamus. Outward from the just described bundle there is another direct path that arises in the ankylosing spondylitis nucleus. Its straight fibers occupy the outermost part of the posterior longitudinal fasciculus and are directed, according to Venderovich and Klosovsky, to the nucleus of the oculomotor nerve. Some of the fibers go further, rise to the posterior commissure and end in the interstitial nucleus and in the optic thalamus.
Thus, in this ascending system There are two pathways of fibers: one is short, ending in the nuclei of the oculomotor nerves, and the other is long, reaching the Darkshevich nucleus, the interstitial nucleus and the optic thalamus.
Besides, in reticularis of the brainstem According to some authors, there are fibers going from the vestibular nuclei to the oculomotor nuclei, since bilateral transection of the posterior longitudinal fasciculi does not relieve mild experimental nystagmus.
Klosovsky in his criticism of the works Spiegel and Lorente de No, without denying the presence of connections between the vestibular and reticular nuclei, is very skeptical about the possibility of connections between these latter and the oculomotor nuclei. In any case, these connections are very insignificant and multi-neuronal and cannot be compared with the powerful, direct vestibular-oculomotor connections through the posterior longitudinal fasciculus.
Above this so-called primary vestibular reflex arc, which contains the vestibular, oculomotor nuclei, nuclear formations in the posterior commissure, as well as all the pathways between them, including the posterior longitudinal fascicles, there are also supravestibular (supratentorial) centers and pathways.
Thus, it is believed, for example, that the vestibular nuclei are connected by pathways to the thalamus optic, and through it to the striatum and cortex.
1 - basilar groove
2 - trapezoid body
3 - bridge base
4 - bridge tire
5 - transverse fibers of the bridge
6 - longitudinal fibers of the bridge
7 - diamond-shaped fossa
8 - superior cerebellar peduncle
9 - reticular formation
10 - medial loop
11 - abducens nerve
12 - facial nerve
13 - vestibulocochlear nerve
14 - glossopharyngeal nerve
15 - vagus nerve
16 - accessory nerve
17 - hypoglossal nerve
Upper olive.
In the bridge tire there is a paired upper olive core, in which part of the auditory fibers switches, and also the nuclei of the reticular formation are located. In the superior olive, auditory information is interrupted for the purpose of processing it. From here descending fibers begin, heading into the inner ear to the receptors.
Vestibular nuclei. Balance system.
The vestibular nuclei are an organ that records changes in body position in space and is located in the inner ear. Excitation of the vestibular nuclei occurs under the influence of an adequate stimulus acting on the vestibular apparatus.
Also, from the vestibular nuclei of the medulla oblongata there is a path to the so-called medial fasciculus, directed towards the spinal cord. This bundle performs an important function: it connects together all the nuclei of the nerves involved in regulating the activity of the muscles of the eyeball. Signals coming from the vestibular nuclei enter the longitudinal medial fasciculus, due to which, when the vestibular apparatus is activated, the phenomenon of nystagmus occurs (involuntary oscillatory movements of the eyes with a high frequency (up to several hundred per minute)). Thus, when the vestibular apparatus is irritated, a redistribution of muscle tone occurs and a change in the activity of the muscles of the eyeball occurs, as a result of which the animal is able to maintain balance and direct its gaze in the desired direction.
Neurons of the vestibular nuclei have the ability to respond to changes in the position of the limbs, turns of the body, signals from internal organs, i.e., to synthesize information coming from different sources. At the same time, they provide control and management of various motor reactions.
The most important of these reactions are vestibulospinal, vestibulo-vegetative and vestibuloculomotor. Vestibulospinal influences through the vestibulo-, reticulo- and rubrospinal tracts provide changes in the impulses of neurons at the segmental levels of the spinal cord. In this way, a dynamic redistribution of skeletal muscle tone and reflex reactions necessary to maintain balance are carried out. The cerebellum is responsible for the phasic nature of these reactions: after its removal, vestibulospinal influences become predominantly tonic. During voluntary movements, vestibular influences on the spinal cord are weakened.
The central axons of the primary sensory neurons of the vestibular ganglion terminate on the neurons of the vestibular nuclei. These nuclei represent a single functional complex, which combines afferent information from the vestibular ganglia and from proprioceptors; this afferentation determines the nature of the activity of neurons in the vestibular nuclei.
The fibers of the vestibular nerve divide before approaching certain cell groups of the vestibular nuclei, where the second neurons begin. Some of its fibers transmit impulses directly, without switching to the cerebellum. The vestibular nuclei have a two-way connection with the cerebellum.
The vestibular nuclei complex includes:
Superior vestibular nucleus (Bechterew's nucleus)
- Lateral vestibular nucleus (Deiters nucleus)
- Medial vestibular nucleus (Schwalbe nucleus)
- Inferior vestibular nucleus (Roller's nucleus)
Vestibular neurons send their fibers to:
-spinal cord
-trunk
-cerebellum
Projections above the cerebellum have not been proven, i.e.the representation of the vestibular system has not been proven either in the Thalamus or in the cerebral cortex(see first table of lecture 8).
Own bridge cores.
The gray matter of the base of the pons is represented own bridge cores. These nuclei play the role of intermediate centers of communication between the cerebral cortex and the cerebellum, i.e. their neurons receive information and transfer it to the cerebellar cortex. There are a lot of these nuclei (about 20 thousand), these are small inclusions of gray matter in the white matter (the base of the pons is represented by both white and gray matter, in contrast to the base of the medulla oblongata).
Bridge conductive paths:
-corticospinal fibers
-corticomontine fibers
-corticobulbar fibers
Red core.
The red nucleus is a structure of the midbrain, located symmetrically in the thickness of the cerebral peduncles under the central gray matter. It is a large accumulation of nerve cells, which, along with other formations, plays a key role in the extrapyramidal (automatic, without the participation of consciousness) system. The red nucleus is closely connected with the structures of the cerebellum.
The neurons of this nucleus receive information from the cerebral cortex and cerebellum, that is, all information about the position of the body in space, the state of the muscular system, and skin. The influence on alpha motor neurons of the spinal cord is carried out using the rubrospinal tract. The rubrospinal tract begins from the cells of the red nucleus located in the cortex of the cerebral peduncles. Activation of neurons in the red nucleus causes excitatory postsynaptic potentials in flexor motor neurons, and inhibitory postsynaptic potentials in extensor motor neurons. In this respect, the rubrospinal tract is similar to the corticospinal tract.
Tectal area:
- a general startle reaction (a sharp increase in the modality of any stimulus: there was nothing and suddenly a sharp impact on the sensory organ);
- orienting reflex - orients to the source of the stimulus, it is suppressed (when the stimulus is repeated, if it is insignificant, it is suppressed (we stop responding to it), suppression requires the participation of the cerebral cortex; it is based on the sentry reflex;