Under normal conditions, a person breathes ordinary air, which has a relatively constant composition (Table 1). There is always less oxygen and more carbon dioxide in the exhaled air. Alveolar air contains the least oxygen and the most carbon dioxide. The difference in the composition of alveolar and exhaled air is explained by the fact that the latter is a mixture of dead space air and alveolar air.
Alveolar air is the internal gas environment of the body. The gas composition of arterial blood depends on its composition. Regulatory mechanisms maintain the constancy of the composition of alveolar air. The composition of alveolar air during quiet breathing depends little on the phases of inhalation and exhalation. For example, the carbon dioxide content at the end of inhalation is only 0.2-0.3% less than at the end of exhalation, since with each inhalation only 1/7 of the alveolar air is renewed. In addition, it occurs continuously during inhalation and exhalation, which helps to equalize the composition of alveolar air. With deep breathing, the dependence of the composition of alveolar air on inhalation and exhalation increases.
Table 1. Air composition (in%)
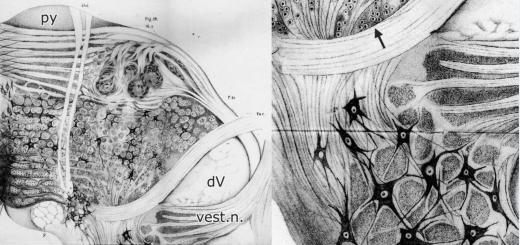
Gas exchange in the lungs occurs as a result of the diffusion of oxygen from the alveolar air into the blood (about 500 liters per day) and carbon dioxide from the blood into the alveolar air (about 430 liters per day). Diffusion occurs due to the difference in the partial pressure of these gases in the alveolar air and their tension in the blood.
Gas partial pressure: concept and formula
Gas partial pressure in a gas mixture is proportional to the percentage of gas and the total pressure of the mixture:
For air: P atmospheric = 760 mm Hg. Art.; C oxygen = 20.95%.
It depends on the nature of the gas. The entire gas mixture of atmospheric air is taken as 100%; it has a pressure of 760 mm Hg. Art., and part of the gas (oxygen - 20.95%) is taken as X. Hence the partial pressure of oxygen in the air mixture is 159 mm Hg. Art. When calculating the partial pressure of gases in the alveolar air, it is necessary to take into account that it is saturated with water vapor, the pressure of which is 47 mm Hg. Art. Consequently, the proportion of the gas mixture that is part of the alveolar air does not account for a pressure of 760 mm Hg. Art., and 760 - 47 = 713 mm Hg. Art. This pressure is taken as 100%. From here it is easy to calculate that the partial pressure of oxygen, which is contained in the alveolar air in the amount of 14.3%, will be equal to 102 mm Hg. Art.; Accordingly, the calculation of the partial pressure of carbon dioxide shows that it is equal to 40 mm Hg. Art.
The partial pressure of oxygen and carbon dioxide in the alveolar air is the force with which the molecules of these gases strive to penetrate the alveolar membrane into the blood.
Diffusion of gases through a barrier obeys Fick's law; Since the membrane thickness and diffusion area are the same, diffusion depends on the diffusion coefficient and pressure gradient:
![]()
Gas Q- volume of gas passing through the tissue per unit time; S - fabric area; DK - gas diffusion coefficient; (P 1, - P 2) - gas partial pressure gradient; T is the thickness of the tissue barrier.
Considering that in the alveolar blood flowing to the lungs, the partial oxygen tension is 40 mmHg. Art., and carbon dioxide - 46-48 mm Hg. Art., then the pressure gradient determining the diffusion of gases in the lungs will be: for oxygen 102 - 40 = 62 mm Hg. Art.; for carbon dioxide 40 - 46(48) = minus 6 - minus 8 mm Hg. Art. Since the diffusion coefficient of carbon dioxide is 25 times greater than that of oxygen, carbon dioxide moves more actively from the capillaries into the alveoli than oxygen in the opposite direction.
In the blood, gases are in a dissolved (free) and chemically bound state. Only dissolved gas molecules participate in diffusion. The amount of gas dissolving in a liquid depends on:
- on the composition of the liquid;
- volume and pressure of gas in liquid;
- liquid temperature;
- nature of the gas under study.
The higher the pressure and temperature of a given gas, the more gas dissolves in the liquid. At a pressure of 760 mm Hg. Art. and a temperature of 38 °C, 2.2% oxygen and 5.1% carbon dioxide dissolve in 1 ml of blood.
The dissolution of a gas in a liquid continues until a dynamic equilibrium occurs between the number of gas molecules dissolving and escaping into the gaseous medium. The force with which molecules of a dissolved gas tend to escape into a gaseous medium is called tension of gas in liquid. Thus, at equilibrium, the gas tension is equal to the partial pressure of the gas in the liquid.
If the partial pressure of a gas is higher than its voltage, then the gas will dissolve. If the partial pressure of a gas is lower than its voltage, then the gas will leave the solution into the gaseous environment.
The partial pressure and tension of oxygen and carbon dioxide in the lungs are given in table. 2.
Table 2. Partial pressure and tension of oxygen and carbon dioxide in the lungs (mm Hg)
Oxygen diffusion is ensured by the difference in partial pressures in the alveoli and blood, which is equal to 62 mm Hg. Art., and for carbon dioxide it is only about 6 mm Hg. Art. The time of blood flow through the capillaries of the small circle (on average 0.7 s) is sufficient for almost complete equalization of the partial pressure and tension of gases: oxygen dissolves in the blood, and carbon dioxide passes into the alveolar air. The transition of carbon dioxide into the alveolar air at a relatively small pressure difference is explained by the high diffusion capacity of the lungs for this gas.
PaO2, along with two other quantities (paCO2 and pH), constitute the concept of “blood gases” (Arterial blood gases - ABG(s)). The paO2 value depends on many parameters, the main ones being the patient’s age and altitude (partial pressure of O2 in atmospheric air). Thus, the pO2 value must be interpreted individually for each patient.
Accurate results for ABGs depend on sample collection, processing, and actual analysis. Clinically important errors can occur at any of these stages, but blood gas measurements are particularly vulnerable to errors occurring before analysis. The most common problems include
- collection of non-arterial (mixed or venous) blood;
- presence of air bubbles in the sample;
- insufficient or excessive amount of anticoagulant in the sample;
- delay in the analysis and storage of the sample during this time uncooled.
A proper blood sample for ABG analysis typically contains 1-3 ml of arterial blood collected anaerobically from a peripheral artery into a special plastic container using a small bore needle. Any air bubbles that may be introduced during sampling must be removed immediately. The air in the room has a paO2 of about 150 mm Hg. (at sea level) and paCO2 is almost zero. Thus, air bubbles that mix with arterial blood shift (increase) paO2 to 150 mm Hg. and reduce (reduce) paCO2.
If heparin is used as an anticoagulant and the collection is made with a syringe rather than a special container, the pH of heparin, which is approximately 7.0, should be taken into account. Thus, excess heparin can change all three ABG values (paO2, paCO2, pH). A very small amount of heparin is needed to prevent clotting; 0.05 - 0.10 ml of dilute heparin solution (1000 U/ml) will counteract the clotting of approximately 1 ml of blood without affecting pH, paO2, paCO2. After flushing the syringe with heparin, a sufficient amount of it usually remains in the dead space of the syringe and needle, which is sufficient for anticoagulation without distorting the ABG values.
After collection, the sample must be analyzed as soon as possible. If a delay of more than 10 minutes occurs, the sample should be immersed in an ice container. Leukocytes and platelets continue to consume oxygen in the sample after collection, and can cause a significant drop in paO2 when stored for long periods at room temperature, especially under conditions of leukocytosis or thrombocytosis. Cooling will prevent any clinically important changes for at least 1 hour by reducing the metabolic activity of these cells.
A decrease in the partial pressure of oxygen in the inhaled air leads to an even lower level in the alveoli and outflowing blood. If plains dwellers climb mountains, hypoxia increases their ventilation by stimulating arterial chemoreceptors. The body responds with adaptive reactions, the purpose of which is to improve the supply of O2 to tissues. Changes in breathing during high-altitude hypoxia vary from person to person. The external respiration reactions that occur in all cases are determined by a number of factors: 1) the speed with which hypoxia develops; 2) degree of O2 consumption (rest or physical activity); 3) duration of hypoxic exposure.
The most important compensatory response to hypoxia is hyperventilation. The initial hypoxic stimulation of respiration, which occurs when rising to altitude, leads to the leaching of CO 2 from the blood and the development of respiratory alkalosis. This in turn causes an increase in the pH of the extracellular fluid of the brain. Central chemoreceptors respond to such a pH shift in the cerebrospinal fluid of the brain by a sharp decrease in their activity, which inhibits the neurons of the respiratory center so much that it becomes insensitive to stimuli emanating from peripheral chemoreceptors. Quite quickly, hyperpnea gives way to involuntary hypoventilation, despite persistent hypoxemia. Such a decrease in the function of the respiratory center increases the degree of hypoxic state of the body, which is extremely dangerous, primarily for the neurons of the cerebral cortex.
With acclimatization to high-altitude conditions, physiological mechanisms adapt to hypoxia. After staying for several days or weeks at altitude, as a rule, respiratory alkalosis is compensated by the release of HCO 3 by the kidneys, due to which part of the inhibitory effect on alveolar hyperventilation disappears and hyperventilation intensifies. Acclimatization also causes an increase in hemoglobin concentration due to increased hypoxic stimulation of erythropoietin by the kidneys. Thus, among Andean residents who constantly live at an altitude of 5000 m, the concentration of hemoglobin in the blood is 200 g/l. The main means of adaptation to hypoxia are: 1) a significant increase in pulmonary ventilation; 2) increase in the number of red blood cells; 3) increase in the diffusion capacity of the lungs; 4) increased vascularization of peripheral tissues; 5) increasing the ability of tissue cells to use oxygen, despite low pO 2.
Some people develop an acute pathological condition when rapidly ascending to high altitudes ( acute mountain sickness and high-altitude pulmonary edema). Since the central nervous system has the highest sensitivity to hypoxia of all organs, neurological disorders are the first to occur when climbing to high altitudes. When rising to altitude, symptoms such as headache, fatigue, and nausea may develop acutely. Pulmonary edema often occurs. Below 4500 m, such severe disturbances occur less frequently, although minor functional deviations occur. Depending on the individual characteristics of the body and its ability to acclimatize, a person is able to reach great heights.
Control questions
1. How do the parameters of barometric pressure and partial pressure of oxygen change with increasing altitude?
2. What adaptive reactions occur when rising to a height?
3. How does acclimatization to high mountain conditions occur?
4. How does acute mountain sickness manifest?
Breathing when diving to depth
When performing underwater work, a diver breathes under pressure 1 atm higher than atmospheric pressure. for every 10 m of dive. About 4/5 of the air is nitrogen. At sea level pressure, nitrogen has no significant effect on the body, but at high pressure it can cause varying degrees of narcosis. The first signs of mild anesthesia appear at a depth of about 37 m, if the diver remains at depth for an hour or more and breathes compressed air. With a long stay at a depth of more than 76 m (pressure 8.5 atm.), nitrogen narcosis usually develops, the manifestations of which are similar to alcohol intoxication. If a person inhales air of normal composition, then nitrogen dissolves in adipose tissue. Diffusion of nitrogen from tissue occurs slowly, so the diver's ascent to the surface must be very slow. Otherwise, intravascular formation of nitrogen bubbles is possible (the blood “boils”) with severe damage to the central nervous system, organs of vision, hearing, and severe pain in the joints. There is a so-called decompression sickness. To treat the victim, it is necessary to place him back in a high-pressure environment. Gradual decompression may last several hours or days.
The likelihood of decompression sickness can be significantly reduced by breathing special gas mixtures, such as an oxygen-helium mixture. This is due to the fact that the solubility of helium is less than that of nitrogen, and it diffuses faster from tissues, since its molecular weight is 7 times less than that of nitrogen. In addition, this mixture has a lower density, so the work spent on external respiration is reduced.
Control questions
5. How do barometric pressure and partial pressure of oxygen change with increasing altitude?
6. What adaptive reactions occur when rising to a height?
7. How does acclimatization to high mountain conditions occur?
8. How does acute mountain sickness manifest?
7.3 Test tasks and situational task
Choose one correct answer.
41. IF A PERSON DIVES WITHOUT SPECIAL EQUIPMENT WITH PRELIMINARY HYPERVENTILATION, THE CAUSE OF SUDDEN LOSS OF CONSCIOUSNESS MAY BE INCREASING
1) asphyxia
2) hypoxia
3) hyperoxia
4) hypercapnia
42. WHEN DIVING UNDER WATER WITH A MASK AND SNORKEL, YOU CANNOT INCREASE THE LENGTH OF THE STANDARD TUBE (30-35 cm) BECAUSE
1) the occurrence of a pressure gradient between air pressure in the alveoli and water pressure on the chest
2) the danger of hypercapnia
3) danger of hypoxia
4) increasing the volume of dead space
Situational task 8
Champion divers dive to depths of up to 100 m without scuba gear and return to the surface in 4-5 minutes. Why don't they get decompression sickness?
8. Standards of answers to test tasks and situational tasks
Sample answers to test tasks:
Standard answers to situational problems:
Solution to situational problem No. 1:
If we are talking about natural breathing, then the first one is right. The breathing mechanism is suction. But, if we mean artificial respiration, then the second one is right, since the mechanism here is a pressure one.
Solution to situational problem No. 2:
For effective gas exchange, a certain ratio between ventilation and blood flow in the vessels of the lungs is necessary. Consequently, these people had differences in blood flow values.
Solution to situational problem No. 3:
In the blood, oxygen exists in two states: physically dissolved and bound to hemoglobin. If hemoglobin does not work well, then only dissolved oxygen remains. But there is very little of it. This means it is necessary to increase its quantity. This is achieved through hyperbaric oxygen therapy (the patient is placed in a chamber with high oxygen pressure).
Solution to situational problem No. 4:
Malate is oxidized by the NAD-dependent enzyme malate dehydrogenase (mitochondrial fraction). Moreover, during the oxidation of one malate molecule, one NADH·H + molecule is formed, which enters the complete electron transfer chain with the formation of three ATP molecules from three ADP molecules. As you know, ADP is an activator of the respiratory chain, and ATP is an inhibitor. ADP in relation to malate is obviously in short supply. This leads to the fact that the activator (ADP) disappears from the system and the inhibitor (ATP) appears, which, in turn, leads to the stop of the respiratory chain and the absorption of oxygen. Hexokinase catalyzes the transfer of a phosphate group from ATP to glucose to form glucose-6-phosphate and ADP. Thus, when this enzyme operates in the system, the inhibitor (ATP) is consumed and the activator (ADP) appears, so the respiratory chain resumes its work.
Solution to situational problem No. 5:
The enzyme succinate dehydrogenase, which catalyzes the oxidation of succinate, belongs to FAD-dependent dehydrogenases. As you know, FADN 2 ensures the supply of hydrogen to the shortened electron transport chain, during which 2 ATP molecules are formed. Amobarbital blocks the respiratory chain at the level of the 1st coupling of respiration and phosphorylation and does not affect the oxidation of succinate.
Solution to situational problem No. 6:
If the umbilical cord is clamped very slowly, the carbon dioxide content in the blood will correspondingly increase very slowly and the neurons of the respiratory center will not be able to excite. The first breath will never happen.
Solution to situational problem No. 7:
Carbon dioxide plays a leading role in excitation of neurons of the respiratory center. In an agonal state, the excitability of the neurons of the respiratory center sharply decreases and therefore they cannot be excited by the action of normal amounts of carbon dioxide. After several respiratory cycles, a pause occurs, during which significant amounts of carbon dioxide accumulate. Now they can already excite the respiratory center. Several inhalations and exhalations occur, the amount of carbon dioxide decreases, a pause occurs again, etc. If the patient's condition cannot be improved, death is inevitable.
Solution to situational problem No. 8:
A diver at great depths breathes high-pressure air. Therefore, the solubility of gases in the blood increases significantly. Nitrogen is not consumed in the body. Therefore, when it rises quickly, its increased pressure quickly decreases, and it is rapidly released from the blood in the form of bubbles, which leads to embolism. The diver does not breathe at all during the dive. When raised quickly, nothing bad happens.
Annex 1
Table 1
Name of pulmonary ventilation indicators in Russian and English
| Name of the indicator in Russian | Accepted abbreviation | Indicator name in English | Accepted abbreviation |
| Vital capacity of the lungs | vital capacity | Vital capacity | V.C. |
| Tidal volume | BEFORE | Tidal volume | TV |
| Inspiratory reserve volume | District Department of Internal Affairs | Inspiratory reserve volume | IRV |
| Expiratory reserve volume | ROvyd | Expiratory reserve volume | ERV |
| Maximum ventilation | MVL | Maximum voluntary ventilation | M.W. |
| Forced vital capacity | FVC | Forced vital capacity | FVC |
| Forced expiratory volume in the first second | FEV1 | Forced expiratory volume 1 sec | FEV1 |
| Tiffno index | IT, or FEV1/VC% | FEV1% = FEV1/VC% | |
| Maximum flow rate at the moment of exhalation 25% FVC remaining in the lungs | MOS25 | Maximum expiratory flow 25% FVC | MEF25 |
| Forced expiratory flow 75% FVC | FEF75 | ||
| Maximum flow rate at the moment of exhalation of 50% FVC remaining in the lungs | MOS50 | Maximum expiratory flow 50% FVC | MEF50 |
| Forced expiratory flow 50% FVC | FEF50 | ||
| Maximum flow rate at the moment of exhalation 75% FVC remaining in the lungs | MOS75 | Maximum expiratory flow 75% FVC | MEF75 |
| Forced expiratory flow 25% FVC | FEF25 | ||
| Average expiratory volumetric flow rate in the range from 25% to 75% FVC | SOS25-75 | Maximum expiratory flow 25-75% FVC | MEF25-75 |
| Forced expiratory flow 25-75% FVC | FEF25-75 |
Appendix 2
BASIC BREATHING PARAMETERS
Vital Capacity (VC = Vital Capacity) - vital capacity of the lungs(the volume of air that leaves the lungs when exhaling as deeply as possible after inhaling as deeply as possible)
IRV (IRV = inspiratory reserve volume) - inspiratory reserve volume(extra air) is the volume of air that can be inhaled during a maximum inhalation after a normal inhalation
ROvyd (ERV = Expiratory Reserve Volume) - expiratory reserve volume(reserve air) is the volume of air that can be exhaled during a maximum exhalation after a normal exhalation
EB (IC = inspiratory capacity) - inhalation capacity- actual sum of tidal volume and inspiratory reserve volume (EB = DO + ROvd)
FOEL (FRC = functional residual capacity) - functional residual capacity of the lungs. This is the volume of air in the lungs of a patient at rest, in a position where normal exhalation is completed and the glottis is open. FOEL is the sum of the expiratory reserve volume and residual air (FOEL = ROV + OB). This parameter can be measured using one of two methods: helium dilution or body plethysmography. Spirometry does not measure FUEL, so the value of this parameter must be entered manually.
OV (RV = residual volume) - residual air(another name is RVL, residual lung volume) is the volume of air that remains in the lungs after maximum exhalation. Residual volume cannot be determined using spirometry alone; this requires additional measurements of lung volume (using the helium dilution method or body plethysmography).
TLC (TLC = total lung capacity) - total lung capacity(the volume of air in the lungs after taking the deepest breath possible). VEL = vital capacity + ov
1.8 Partial tension of oxygen in the blood
PaO2 is the partial tension of oxygen in arterial blood. This is the tension of physically distributed oxygen in arterial blood plasma under the influence of a partial pressure equal to 100 mm Hg (PaO2 = 100 mm Hg). Every 100 ml of plasma contains 0.3 ml of oxygen. The O2 content in the arterial blood of trained athletes under resting conditions does not differ from its content in non-athletes. During physical activity, an accelerated breakdown of oxyhemoglobin occurs in the arterial blood flowing to the muscles with the release of free O2, so PaO2 increases
PвO2 is the partial tension of oxygen in venous blood. This is the tension of physically dissolved oxygen in the plasma of venous blood flowing from the tissue (muscle). Characterizes the tissue's ability to utilize oxygen. At rest it is 40-50 mm Hg. At maximum work, due to intensive utilization of O2 by working muscles, it decreases to 10-20 mm Hg. Art.
The difference between PaO2 and PvO2 is the value of ABP-O2 - the arterial-venous difference in oxygen. Characterizes the tissue's ability to utilize oxygen. ABP-O2 is the difference between the oxygen content in arterial blood released into the systemic arteries from the left ventricle and in venous blood flowing to the right atrium.
With the development of aerobic endurance, pronounced sarcoplasmic hypertrophy of skeletal muscles occurs, which leads to a decrease in oxygen in the venous blood (PbO2), and a corresponding increase in ABP-O2. So, if at rest PbO2 in men and women is 30 mm Hg, then after endurance exercise in untrained men PbO2 = 13 mm Hg, in untrained women 14 mm Hg. Accordingly, in trained men and women - 10 and 11 mm Hg. In women, the content of hemoglobin, bcc and oxygen content in arterial blood is lower, therefore, with equal oxygen content in venous blood, the total systemic ABP-O2 in women is less. At rest, it is equal to 5.8 ml of O2 per 100 ml of blood, versus 6.5 in men. After completing the exercise, untrained women had ABP-O2 = 11.1 ml O2/100 ml of blood, versus 14 in untrained men. As a result of training, ABP-O2 increases in both women and men as a result of a decrease in the oxygen content in the venous blood (12.8 and 15.5, respectively).
According to Fick's formula (PO2(MPC) = SV*ABP-O2), the product of SV by AVR-O2 determines the maximum oxygen consumption and is an important indicator of aerobic endurance. Endurance athletes use their oxygen transport capabilities more efficiently because they use more oxygen contained in each milliliter of blood than untrained people.
1.9 The influence of health training on the hemodynamics of the body
As a result of health training, the functionality of the cardiovascular system increases. There is an economization of the work of the heart at rest and an increase in the reserve capabilities of the circulatory apparatus during muscle activity. One of the most important effects of physical training is a decrease in heart rate at rest (bradycardia) as a manifestation of economization of cardiac activity and lower myocardial oxygen demand. Increasing the duration of the diastole (relaxation) phase provides greater blood flow and a better supply of oxygen to the heart muscle. In people with bradycardia, cases of coronary heart disease (CHD) are detected much less frequently than in people with a rapid pulse. It is believed that an increase in heart rate at rest by 15 beats/min increases the risk of sudden death from a heart attack by 70%. The same pattern is observed with muscle activity.
When performing a standard load on a bicycle ergometer in trained men, the volume of coronary blood flow is almost 2 times less than in untrained men (140 versus 260 ml/min per 100 g of myocardial tissue), and the myocardial oxygen demand is correspondingly 2 times less (20 versus 40 ml /min per 100g tissue). Thus, with an increase in the level of training, the myocardial oxygen demand decreases both at rest and at submaximal loads, which indicates economization of cardiac activity. As training increases and myocardial oxygen demand decreases, the level of threshold load that the subject can perform without the threat of myocardial ischemia and an attack of angina increases.
The most pronounced increase in the reserve capabilities of the circulatory system during intense muscular activity is: an increase in maximum heart rate, CO and MV, ABP-O2, a decrease in total peripheral vascular resistance, which facilitates the mechanical work of the heart and increases its productivity. Adaptation of the peripheral blood circulation comes down to an increase in muscle blood flow under extreme loads (maximum 100 times), an arteriovenous difference in oxygen, the density of the capillary bed in working muscles, an increase in the concentration of myoglobin and an increase in the activity of oxidative enzymes.
An increase in fibrinolytic activity of the blood during health-improving training (maximum 6 times) and a decrease in the tone of the sympathetic nervous system also play a protective role in the prevention of cardiovascular diseases. As a result, the response to neurohormones decreases under conditions of emotional stress, i.e. The body's resistance to stress increases.
In addition to the pronounced increase in the body's reserve capabilities under the influence of health-improving training, its preventive effect is also extremely important. With increasing training (as the level of physical performance increases), there is a clear decrease in all the main risk factors: cholesterol in the blood, blood pressure and body weight. There are examples when, as UVC increased, the cholesterol content in the blood decreased from 280 to 210 mg, and triglycerides from 168 to 150 mg%. At any age, with the help of training, you can increase aerobic capacity and the level of endurance - indicators of the biological age of the body and its vitality. For example, well-trained middle-aged runners have a maximum possible heart rate that is about 10 beats per minute higher than untrained runners. Physical exercises such as walking and running (3 hours per week) already after 10-12 weeks lead to an increase in VO2 max by 10-15%.
Thus, the health-improving effect of mass physical education is associated primarily with an increase in the aerobic capabilities of the body, the level of general endurance and physical performance. Increased performance is accompanied by a preventive effect against risk factors for cardiovascular diseases: a decrease in body weight and fat mass, cholesterol and triglycerides in the blood, a decrease in blood pressure and heart rate. In addition, regular physical training can significantly slow down the development of age-related changes in physiological functions, as well as degenerative changes in various organs and systems (including delay and reverse development of atherosclerosis). Performing physical exercises has a positive effect on all parts of the musculoskeletal system, preventing the development of degenerative changes associated with age and physical inactivity. The mineralization of bone tissue and calcium content in the body increases, which prevents the development of osteoporosis. The flow of lymph to the articular cartilage and intervertebral discs increases, which is the best means of preventing arthrosis and osteochondrosis. All these data indicate the invaluable positive impact of health-improving physical education on the human body.
Conclusion
This course work examined the main hemodynamic characteristics and their changes during physical activity. Brief conclusions are summarized in Table 10.
Table10. Basic hemodynamic characteristics
| Definition | Characteristic. | Training effect | |
| Heart rate | Heart rate - heart rate contractions per minute (pulse rate). | Resting heart rate average. For men - 60 beats/min, for women - 75, for trained ones. husband. -55, for outstanding athletes - 50 beats/min. Minimum The recorded resting heart rate for athletes is 21 beats/min. Heart rate max avg. for men 200 beats/min, for trained ones - 195, for super athletes -190 beats/min (exercise max. aerobic power), 180 beats/m (max. anaerobic power), max heart rate for untrained women - 205 beats/min, for athletes - 195 beats/min. | A decrease in heart rate (bradycardia) is an effect of endurance training and leads to a decrease in myocardial oxygen demand. |
| CO | CO=SV/HR The amount of blood ejected by each ventricle of the heart during one contraction. | The CO2 of rest in untrained men is on average 70-80 ml, in trained men - 90 ml, in outstanding athletes - 100-120 ml. At maximum aerobic load, COmax in untrained young men is 120-130 ml, in trained ones - 150, in outstanding athletes - 190-210 ml. COmax for untrained women is 90 ml, for outstanding stayers it is 140-150 ml. | An increase in CO as a result of exercise is a sign of increased heart efficiency. |
| SV or MOK or Q | CO=CO*HR SV=PO2/AVR-O2 Amount of blood ejected by the heart in 1 minute IOC - Volume of blood passing through. through the bloodstream vessels per unit time Q=P/R- Blood flow | SV at rest in men = 4-5 l/min, in women - 3-5 l/min. Average SVmax in untrained men is 24 l/min, in super athletes (endurance training) and those with a large heart volume (1200-1300 ml) - more than 30 l/min - for skiers, SVmax = 38–42 l/min. In untrained women, SV-18l/min. For outstanding athletes, CBmax = 28-30. Basic equation of hemodynamics P-blood pressure, R-vascular resistance. | One of the main effects of endurance training is an increase in CBmax. The increase in CO is not due to heart rate, but due to CO |
| HELL | SBP - SystolicBP - maximum blood pressure on the aortic wall achieved at the moment of SV DBP-DiastolicBP the pressure of the blood with which it returns to the atrium in diastole. | Standards BP-100-129 mm Hg. for max. and 60-79 mm Hg. for the minimum for persons under 39 years of age The upper limit of normal systolic pressure from 21 to 60 years of age is 140 mm Hg, for diastolic pressure is 90 mm Hg. With little physical activity, BPmax increases to 130-140 mmHg, with moderate exercise to 140-170, with heavy exercise to 180-200. Administrator, usually with physical the load decreases. For hypertension and physical activity, SADmax = 250 mm Hg. An increase in blood pressure is associated with an increase in R and CO. | Exercising helps lower blood pressure, but blood pressure does not go beyond normal limits. Dynamic loads (endurance exercise) help lower blood pressure, statistical loads (strength exercise) help to raise blood pressure. |
| R | 3.14*R^4-Vascular or peripheral. resistant | Depends on L-length of the vessel, n-blood viscosity, R-radius of the vessel; 3.14 is the number Pi. | Redistribution of blood flow, increased capillarization, slowing down the speed of blood flow in highly trained athletes. |
| BCC | BCC - Circulating blood volume - the total amount of blood located in the blood vessels. | It makes up 5-8% of weight, at rest in women - 4.3 l, in men - 5.5 l. During exercise, the bcc first increases and then decreases by 0.2-0.3 l due to the outflow of part of the plasma from the capillaries into the intercellular space. In women at max. work BCC average = 4 l, for men - 5.2 l. With a load of maximum aerobic power in trained men, BCCavg = 6.42 l. | Increase in blood volume during endurance training. |
| PaO2, PвO2 | PaO2, PвO2 - Partial tension of oxygen in arterial or venous blood. Partial pressure. PaO2-PвO2 =АВР-О2 arterial-venous difference in oxygen | PaO2-100mmHg.PbO2pok-40-50mmHg.PbO2max.work=10-20mmHg. If PbO2 at rest in men and women is 30 mm Hg, then after endurance exercise in untrained men PbO2 = 13 mm Hg, women 14 mm Hg. Accordingly, in trained men and women - 10 and 11 mm Hg. AVR-O2 at rest = 5.8 mlO2/100 ml of blood, versus 6.5 in men. After exercise, in untrained women, AVR-O2 = 11.1 mlO2/100 ml of blood, versus 14 in men. As a result of training, ABP-O2 in women was 12.8, in men - 15.51 ml O2 / 100 ml of blood. | Sarcoplasmic hypertrophy of skeletal muscles leads to a decrease in the oxygen content in the venous blood PvO2 and an increase in ABP-O2. Consequently, the BMD increases. |
Column 3 provides a brief description of the studied quantities and their limit values.
The degree of change in hemodynamic parameters during physical activity depends on the initial values at rest. Physical activity requires a significant increase in the functions of the cardiovascular, respiratory and circulatory systems. Providing working muscles with a sufficient amount of oxygen and removing carbon dioxide from tissues depends on this. The cardiovascular system has a number of mechanisms that allow it to deliver as much blood as possible to the periphery. First of all, these are hemodynamic factors: an increase in heart rate, CO, blood volume, acceleration of blood flow, changes in blood pressure. These indicators are different for representatives of different sports. (According to sports specialization, sprinters train speed, stayers train endurance, weightlifters train strength.)
The use of echocardiography in sports medicine has made it possible to establish differences in the ways of heart adaptation depending on the direction of the training process. In athletes training endurance, cardiac adaptation occurs primarily due to dilatation with slight hypertrophy, and in athletes training strength - due to true myocardial hypertrophy and slight dilatation. With intense physical work, cardiac activity increases. The heart should be trained gradually according to age.
A hemodynamic factor such as changes in blood pressure is very important. The direction of the training process affects blood pressure. Physical loads of a dynamic nature help to reduce it, while statistical loads help to increase it. Hypertension can be caused by physical and emotional stress. A low level of systolic pressure in the pulmonary artery is an indicator of the high state of the cardiovascular system of endurance athletes. It characterizes the potential readiness of the body, in particular hemodynamics, for large and prolonged physical exertion.
The physiological changes in the body caused by endurance training are the same in women as in men. Thus, in the oxygen transport system, maximum indicators (LVmax, SVmax, COmax), lactate concentration at maximum work increase, and HRmax decreases due to increased parasympathetic influences. All this indicates an increase in efficiency and economy, as well as an increase in the reserve capabilities of the oxygen transport system.
The state of the body, both at rest and during exercise, depends on many reasons: external conditions, specific sports (swimming, winter sports, etc.), hereditary factors, gender, age, etc.
The limit to the growth of training effects in each person is genetically predetermined. Even systematic intense physical training cannot increase the body's functional capabilities beyond the limit determined by the genotype. Resting heart rate, heart size, left ventricular wall thickness, myocardial capillarization, and coronary artery wall thickness are influenced by hereditary factors.
It must be borne in mind that physical exercise helps to improve health, improve the biological mechanisms of protective and adaptive reactions, and increase nonspecific resistance to various harmful environmental influences, only under the obligatory condition that the degree of physical activity in these classes is optimal for this particular person. Only the optimal degree of physical activity, corresponding to the capabilities of the person performing it, ensures improved health, physical improvement, prevents the occurrence of a number of diseases and helps to increase life expectancy. Physical activity less than optimal does not give the desired effect, above optimal it becomes excessive, and excessive activity, instead of a healing effect, can cause various diseases and even sudden death from cardiac overstrain. Sports achievements should increase as a result of improved health.
Special mention should be made of the influence of health-improving physical culture on the aging body. Physical education is the main means of delaying age-related deterioration of physical qualities and a decrease in the adaptive abilities of the body in general and the cardiovascular system in particular. Changes in the circulatory system and a decrease in cardiac performance entail a pronounced decrease in the maximum aerobic capabilities of the body, a decrease in the level of physical performance and endurance. The rate of age-related decrease in MOC in the period from 20 to 65 years in untrained men averages 0.5 ml/min/kg, in women - 0.3 ml/min/kg per year. In the period from 20 to 70 years, maximum aerobic performance decreases by almost 2 times - from 45 to 25 ml/kg (or by 10% per decade). Adequate physical training and health-improving physical education classes can significantly stop age-related changes in various functions. Physical labor, physical education and outdoor sports are especially beneficial, while smoking and alcohol abuse are especially harmful to the cardiovascular system.
The above material traces the patterns of changes in the basic hemodynamic characteristics of the body. Simultaneously increasing the level of health and functional state of a person is impossible without the active, widespread and comprehensive use of physical education and sports.
Literature
1. A.S. Zalmanov. The secret wisdom of the human body (Deep medicine). - M.: Nauka, 1966. - 165 p.
2. Sports medicine (Guide for doctors) / edited by A.V. Chogovadze, L.A. Butchenko.-M.: Medicine, 1984.-384 p.
3. Sports physiology: Textbook for the Institute of Physical Education/Ed. Y.M. Kotsa.-M.: Physical education and sports, 1986.-240 p.
4. Dembo A.G. Medical control in sports. - M.: Medicine. 1988. - 288 p.
5. A. M. Tsuzmer, O. L. Petrishina. Human. Anatomy. Physiology. Hygiene.-M.: Education, 1971.-255 p.
6.V.I. Dubrovsky, Rehabilitation in sports. – M.: Physical culture and sport, 1991. – 208 p.
7. Melnichenko E.V. Methodological instructions for the theoretical study of the course “Sports Physiology”. Simferopol. 2003.
8. Grabovskaya E.Yu. Malygina V.I. Melnichenko E.V. Guidelines for the theoretical study of the course “Physiology of muscular activity.” Simferopol.2003
9. Dembo A.G. Current problems of modern sports medicine. - M.: Physical education and sport, 1980. - 295 p.
10.Byleeva L.V. and others. Outdoor games. Textbook for the Institute of Physical Culture. M.: Physical education and sports, 1974.-208 p.
A.S. Zalmanov. The secret wisdom of the human body (Deep Medicine). - Moscow: Nauka, 1966. - C32.
Sports medicine (Guide for doctors) / edited by A.V. Chogovadze, L.A. Butchenko.-M.: Medicine, 1984.-C83.
Sports medicine (Guide for doctors) / edited by A.V. Chogovadze, L.A. Butchenko.-M.: Medicine, 1984.-C76.
Sports physiology: Textbook for the institute of physical education / Ed. Y.M. Kotsa.-M.: Physical education and sports, 1986.-P.87.
Sports physiology: Textbook for the institute of physical education / Ed. Y.M.Kots.-M.: Physical education and sports, 1986.-P.29
Dembo A.G. Medical control in sports. - M.: Medicine. 1988. - C137.
Sports physiology: Textbook for the institute of physical education / Ed. Y.M. Kotsa.-M.: Physical education and sports, 1986.-P.202
Sports medicine (Guide for doctors) / edited by A.V. Chogovadze, L.A. Butchenko.-M.: Medicine, 1984.-C97.
...) and relative (with significant dilatation of the left ventricle with expansion of the aortic opening) insufficiency of the aortic valve. Etiology 1) RL; 2) FROM; 3) syphilitic aortitis; 4) diffuse connective tissue diseases; 5) atherosclerosis of the aorta; 6) injuries; 7) congenital defect. Pathogenesis and changes in hemodynamics. The main pathological process leads to wrinkling (rheumatism, ...

Literary data on the issue being studied; 2) assess morphofunctional indicators in participants of groups of various training orientations at the initial stage; 3) determine the influence of aerobic and anaerobic physical exercises on the morphofunctional capabilities of those involved; 4) conduct a comparative analysis of the indicators studied among group participants in the dynamics of the training process. 2.2...


We did not find an electrocardiographic technique mainly for identifying physiological and pathological changes in the heart, while we did not find any work that would use ECG indicators to determine fitness and the effect of physical activity on changes in heart rate and blood pressure.”12 The analysis of the ECG showed , that at rest the studied values are for gymnasts 15-16 years old...
The gases that make up the breathing air affect the human body depending on the value of their partial (partial) pressure:
where Pg is the partial gas pressure” kgf/cm², mm Hg. st or kPa;
Pa - absolute air pressure, kgf/cm², mmHg. Art. or kPa.
Example 1.2. Atmospheric air contains 78% nitrogen by volume. 21% oxygen and 0.03% carbon dioxide. Determine the partial pressure of these gases on the surface and at a depth of 40 m. Take atmospheric air pressure equal to 1 kgf/cm².
Solution: 1) absolute pressure of compressed air at a depth of 40 m according to (1.2)
2) partial pressure of nitrogen according to (1.3) on the surface
at a depth of 40 m
3) partial pressure of oxygen on the surface
at a depth of 40 m
4) partial pressure of carbon dioxide on the surface
at a depth of 40 m
Consequently, the partial pressure of gases included in the breathing air at a depth of 40 m increased 5 times.
Example 1.3. Based on the data in Example 1.2, determine what percentage of gases should be at a depth of 40 m so that their partial pressure corresponds to normal conditions on the surface.
Solution: 1) nitrogen content in the air at a depth of 40 m, corresponding to the partial pressure on the surface, according to (1.3)

2) oxygen content under the same conditions

3) carbon dioxide content under the same conditions

Consequently, the physiological effect on the body of the gases that make up the breathing air at a depth of 40 m will be the same as on the surface, provided that their percentage content decreases by 5 times.
Nitrogen air begins to have a toxic effect almost at a partial pressure of 5.5 kgf/cm² (550 kPa). Since atmospheric air contains approximately 78% nitrogen, the indicated partial pressure of nitrogen according to (1.3) corresponds to an absolute air pressure of 7 kgf/cm² (immersion depth - 60 m). At this depth, the swimmer becomes agitated, ability to work and attentiveness decrease, orientation becomes difficult, and sometimes dizziness occurs. At great depths (80...100 m), visual and auditory hallucinations often develop. Almost at depths of 80...90 m, a swimmer becomes unable to work, and descent to these depths while breathing air is only possible for a short time.
Oxygen in high concentrations, even under atmospheric pressure, it has a toxic effect on the body. Thus, at a partial pressure of oxygen of 1 kgf/cm² (breathing pure oxygen in atmospheric conditions), inflammatory phenomena develop in the lungs after 72 hours of breathing. When the partial pressure of oxygen is more than 3 kgf/cm², after 15...30 minutes, convulsions occur and the person loses consciousness. Factors predisposing to the occurrence of oxygen poisoning: the content of carbon dioxide in the inhaled air, strenuous physical work, hypothermia or overheating.
With a low partial pressure of oxygen in the inhaled air (below 0.16 kgf/cm²), the blood flowing through the lungs is not completely saturated with oxygen, which leads to a decrease in performance, and in cases of acute oxygen starvation - to loss of consciousness.
Carbon dioxide. Maintaining normal carbon dioxide levels in the body is regulated by the central nervous system, which is very sensitive to its concentration. An increased content of carbon dioxide in the body leads to poisoning, a decreased content leads to a decrease in the breathing rate and stops it (apnea). Under normal conditions, the partial pressure of carbon dioxide in atmospheric air is 0.0003 kgf/cm² (~30 Pa). If the partial pressure of carbon dioxide in the inhaled air increases by more than 0.03 kgf/cm² (-3 kPa), the body will no longer cope with the removal of this gas through increased breathing and blood circulation and severe disorders may occur.
It should be borne in mind that according to (1.3), a partial pressure of 0.03 kgf/cm² on the surface corresponds to a carbon dioxide concentration of 3%, and at a depth of 40 m (absolute pressure 5 kgf/cm²) - 0.6%. An increased content of carbon dioxide in the inhaled air enhances the toxic effect of nitrogen, which can already appear at a depth of 45 m. That is why it is necessary to strictly monitor the content of carbon dioxide in the inhaled air.
Saturation of the body with gases. Being under high pressure entails saturation of the body with gases that dissolve in tissues and organs. At atmospheric pressure on the surface in a human body weighing 70 kg, about 1 liter of nitrogen is dissolved. With increasing pressure, the ability of body tissues to dissolve gases increases in proportion to the absolute air pressure. So, at a depth of 10 m (absolute air pressure for breathing 2 kgf/cm²) 2 liters of nitrogen can already be dissolved in the body, at a depth of 20 m (3 kgf/cm²) - 3 liters of nitrogen, etc.
The degree of saturation of the body with gases depends on their partial pressure, the time spent under pressure, as well as on the speed of blood flow and pulmonary ventilation.
During physical work, the frequency and depth of breathing, as well as the speed of blood flow, increase, so the saturation of the body with gases is directly dependent on the intensity of the submarine swimmer’s physical activity. With the same physical activity, the speed of blood flow and pulmonary ventilation in a trained person increase to a lesser extent than in an untrained person, and the saturation of the body with gases will be different. Therefore, it is necessary to pay attention to increasing the level of physical fitness and the stable functional state of the cardiovascular and respiratory systems.
A decrease in pressure (decompression) causes desaturation of the body from indifferent gas (nitrogen). In this case, excess dissolved gas enters the bloodstream from the tissues and is carried by the blood stream into the lungs, from where it is removed into the environment by diffusion. If you ascend too quickly, gas dissolved in the tissues forms bubbles of various sizes. They can be carried throughout the body by blood flow and cause blockage of blood vessels, which leads to decompression sickness.
Gases formed in the intestines of a submariner while he is under pressure expand upon ascent, which can lead to pain in the abdomen (flatulence). Therefore, it is necessary to ascend from depth to the surface slowly, and in case of a long stay at depth - with stops in accordance with the decompression tables (Appendix 11.8).